Boston Scientific accounts are for healthcare professionals only.

ROTAPRO™ Rotational Atherectomy System
Reimbursement
Configure or select a product to continue to order
- Overview
- Clinical Data
- Product Specifications
- ROTAWIRE DRIVE
- Ordering Information
- Training and Resources
- Reimbursement
Predictable access to severe lesions
Navigate severe calcium with confidence. ROTAPRO ensures reliable access, transforming unpredictable challenges into routine success. It's more than just a crack – achieve optimal lumen gain for confident stent results.
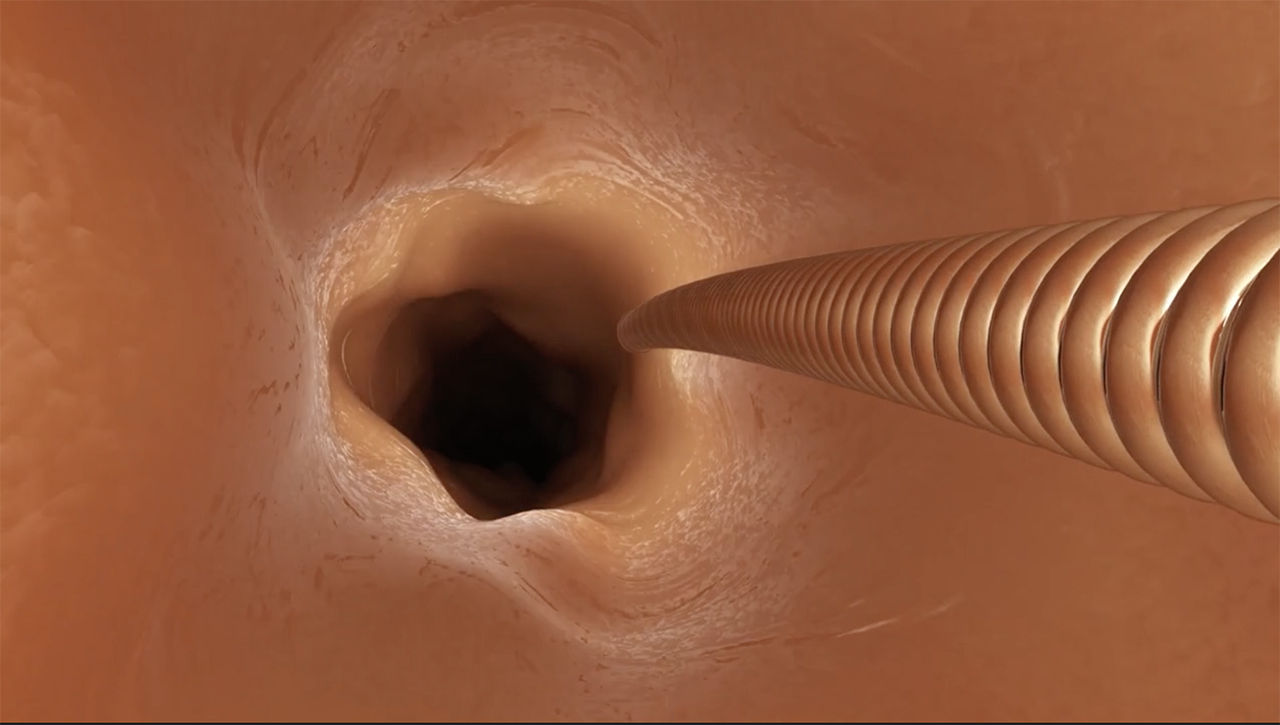
How it works
Why choose ROTAPRO?
ROTAPRO delivers unmatched plaque modification and precision, ensuring predictability and safety when navigating complex lesions.
Ensure access to complex lesions
Carving the way for other PCI treatment tools ROTAPRO provides favorable lumen gain1, plaque modification2 and stent expansion3 in the most heavily calcified lesions.
Proven safety and efficacy
Achieve superior safety and effectiveness in lesion preparation, marked by minimal procedural complications and a high rate of clinical success.4
Precision and control
ROTAPRO’s mechanism of action enhances procedural control and precision, minimizing bleeding risk while ensuring high angiographic success.5
Compatible products
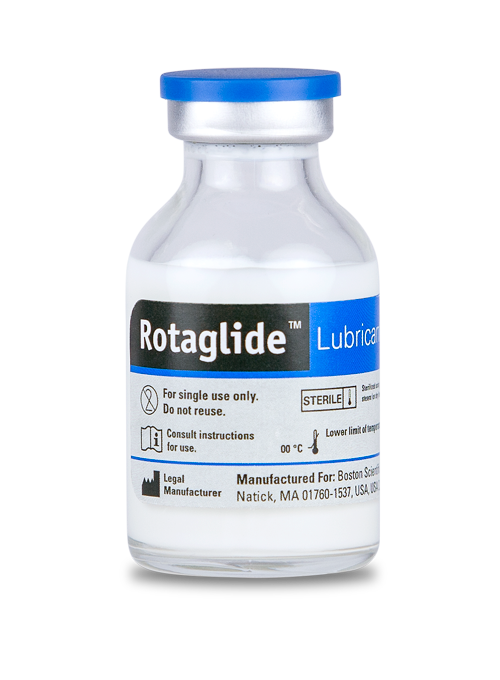
ROTAGLIDE™
ROTAGLIDE is a lipid-based emulsion designed to lubricate the ROTAPRO System.
- Reduces friction and improves tactile feel
- Reduces heat build-up around the ROTAPRO burr
- Reduces sudden drops in RPMs caused by lesion feedback
*Contraindicated if the patient is allergic to eggs or olive oil

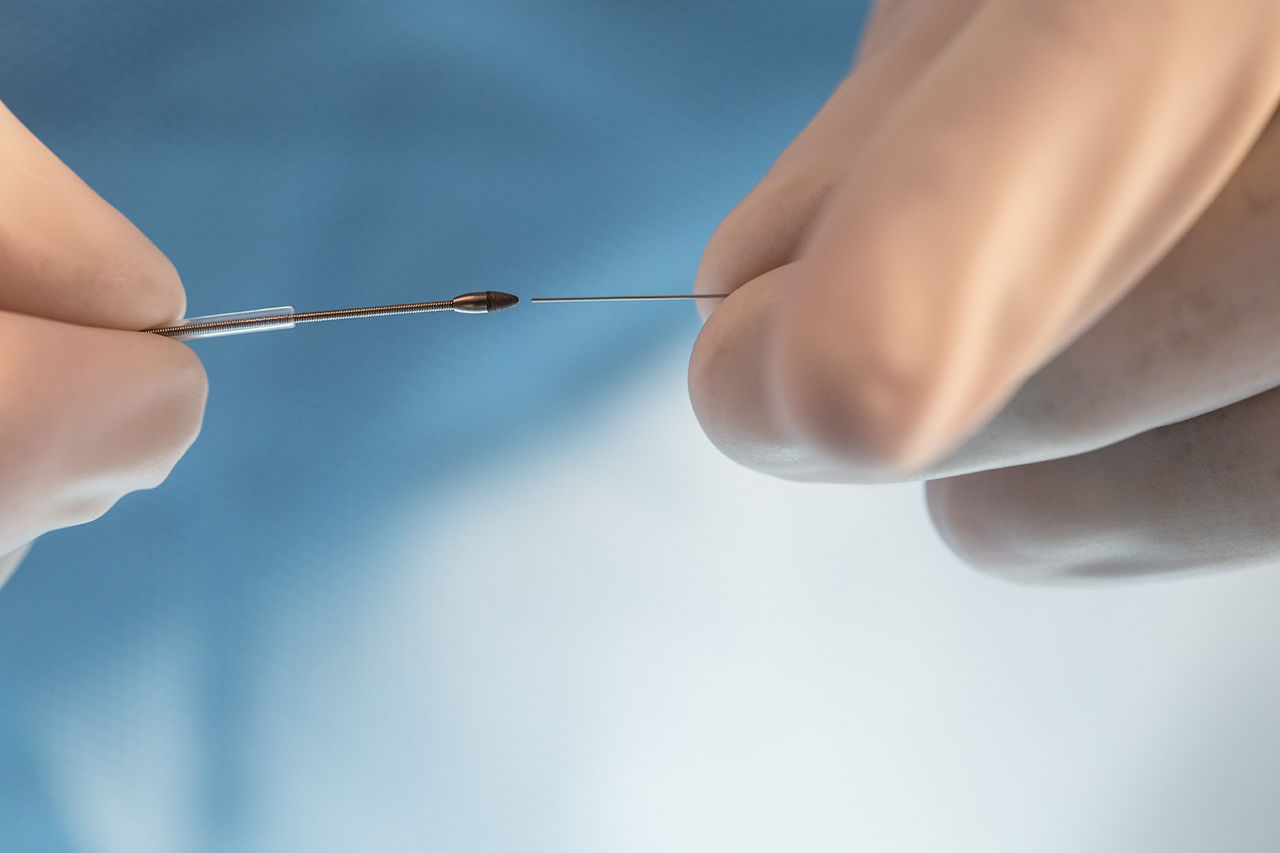
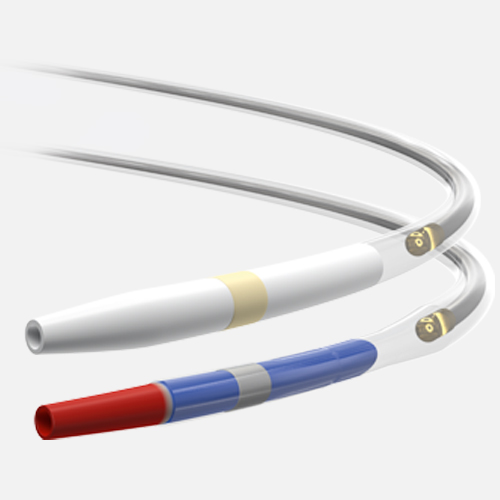
ROTAWIRE Drive™ Guidewire
Features enhanced 1:1 torque transmission for predictable and precise lesion access in tortuous calcified lesions:
- Improved core wire durability- Improved kink and wear resistance
- Highly visible safety tip- .014” platinum coil to provide visibility and added safety
- ASAHITM Core Wire Technology - One-piece stainless steel core wire transmits torque for predictable steering
- Increases procedural efficiency by reducing reliance on wire exchange devices - In a survey of 17 physicians, 12 projected a 3 minute time savings with direct wiring vs utilizing exchange devices
Available in two different wire profiles to provide the support you need.
Subscribe for updates on ROTAPRO
Receive timely updates on significant announcements, exclusive opportunities to engage with peers through educational events, and access to valuable tools to enhance your Modern PCI workflow.
See the vessel
Assess plaque type and severity using the latest imaging and physiology technology. Eliminate guesswork and make clearer treatment decisions.

Prep the vessel
Successful outcomes start with proper lesion assessment and vessel preparation. Achieve optimal lumen gain with our cutting balloon and rotational atherectomy tools.
Treat the vessel
With our innovative stent portfolio and coronary drug-coated balloon technology, you have access to market-leading therapies that will ensure you are able to improve long-term patient outcomes.
The most complete PCI portfolio in the industry
Access the broadest portfolio of dependable, sophisticated PCI devices so you have access to the right tools to see, prepare, and treat coronary artery disease.
An unrivaled clinical legacy
Backed by 30+ years of proven clinical use and superior outcomes. See how ROTAPRO consistently outperforms.
More favorable plaque modification and greater stent expansion compared to orbital atherectomy
The recent investigator-led randomized controlled DIRO study6 directly compared ROTAPRO rotational atherectomy to orbital atherectomy in calcified coronary lesions.
When compared to orbital atherectomy in calcified lesions, rotational atherectomy showed:
More favorable plaque modification (P < 0.01)
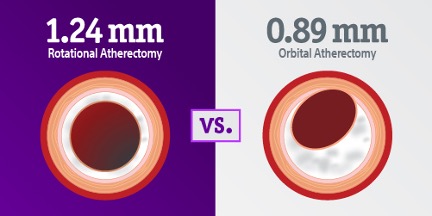
Greater stent expansion (P < 0.02)
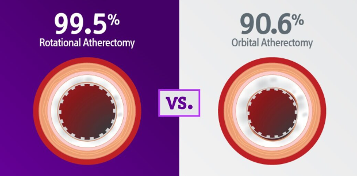
6. Okamoto N, Egami Y, Nohara H, et al. Direct Comparison of Rotational vs Orbital Atherectomy for Calcified Lesions Guided by Optical Coherence Tomography. JACC Cardiovasc Interv. 2023;16(17):2125-2136. doi:10.1016/j.jcin.2023.06.016
ROTACut: Combination strategy results in favorable MSA and ALG
ROTAPRO's unique debulking action not only creates a clear path and optimizes lumen gain where other methods fall short, but also serves as an essential component in effective combination strategies for tackling the most challenging calcium.
7. Allali A, Toelg R, Abdel‐Wahab M, et al. Combined rotational atherectomy and cutting balloon angioplasty prior to drug‐eluting stent implantation in severely calcified coronary lesions: The prepare‐calc‐combo study. Catheterization and Cardiovascular Interventions. 2022;100(6):979-989. doi:10.1002/ccd.30423
Subscribe for updates on ROTAPRO
Receive timely updates on significant announcements, exclusive opportunities to engage with peers through educational events, and access to valuable tools to enhance your Modern PCI workflow.
System components
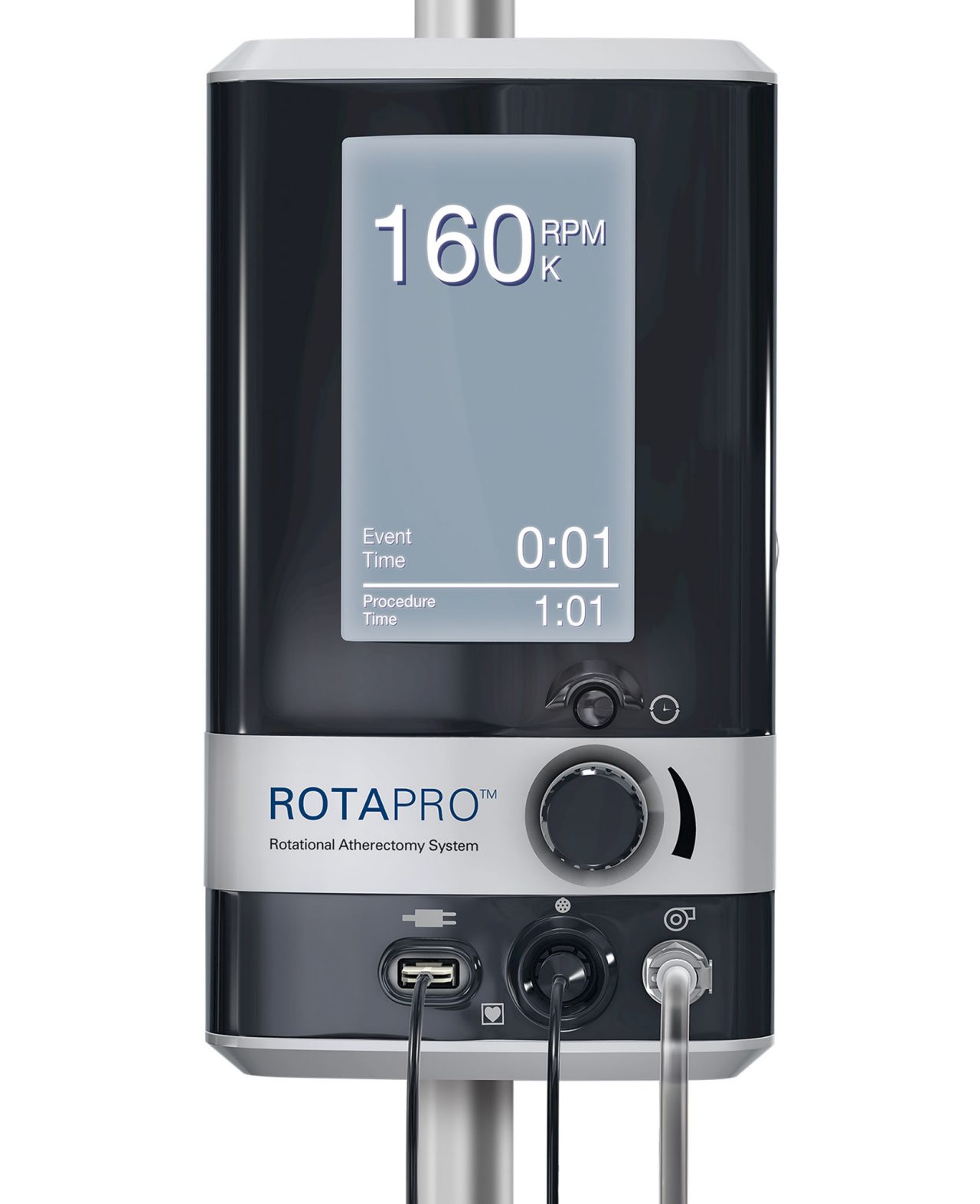
Console
The ROTAPRO Rotational Atherectomy System console regulates the flow of air to the advancer, controlling burr rotation speed. It also monitors and displays burr rotation speed and rotational atherectomy procedural time. The console may be powered by both nitrogen and compressed air.
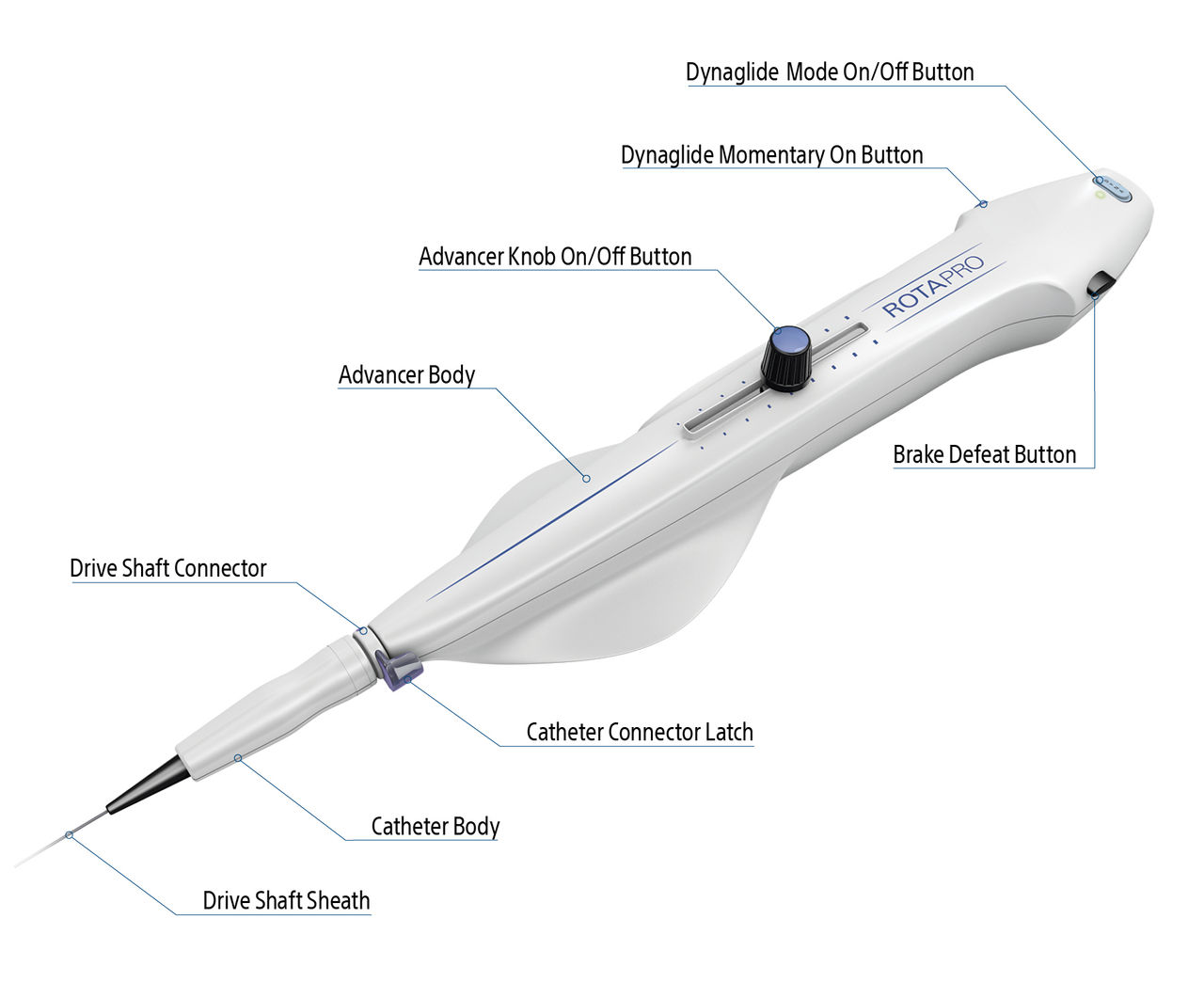
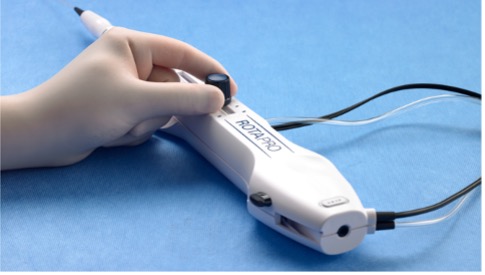
Advancer
The ROTAPRO Rotational Atherectomy system features an advancer which is used to control movement of the burr. The advancer can be purchased individually.
- Easy-to-use Controls – Incorporated on the advancer
- Ergonomic Dynaglide™ Design – Simple system removal
- Hybrid Harness – Improved cable management

Burrs
Achieve predictable lumen size with multiple burr size options.
| ROTAPRO Pre-Connected Burr and Advancing Device | |||||||
|---|---|---|---|---|---|---|---|
| 1.25mm | 1.5mm | 2.75mm | 2.00mm | 2.15mm | 2.25mm | 2.38mm | 2.5mm |

Guidewires
Designs for use with ROTAPRO Rotational Atherectomy System, the ROTAWIRE™ Drive Guidewires provide two types of support depending on procedure requirements.
- Navigate calcified lesions with 1:1 torque through tortuous anatomy
- Have visibility during procedure with 0.014” platinum coil tip design
- Predictability in steering with core wire using Asahi technology
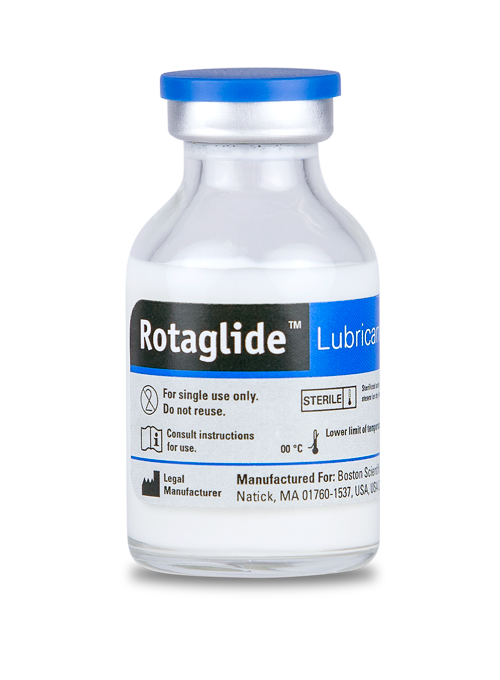
ROTAGLIDE™ Lubricant
ROTAGLIDE is a lipid-based emulsion designed to lubricate the ROTAPRO System.
- Reduces friction and improves tactile feel
- Reduces heat build-up around the ROTAPRO burr
- Reduces sudden drops in RPMs caused by lesion feedback
*Contraindicated if patient is allergic to eggs or olive oil
Subscribe for updates on ROTAPRO
Receive timely updates on significant announcements, exclusive opportunities to engage with peers through educational events, and access to valuable tools to enhance your Modern PCI workflow.
ROTAWIRE™ DRIVE
Enhanced torque transmission for predictable and precise lesion access in calcified lesions.

Why choose ROTAWIRE DRIVE?
Reduce reliance on wire exchange devices, saving procedural time and lowering overall device spend.
Unsurpassed Torque Transmission
Able to navigate calcified lesions with 1:1 torque through tortuous anatomy, providing access for ROTAPRO.
Improved Core Wire Durability
Improved kink resistance and wear resistance compared to the legacy.
Highly Visible Safety Tip
014 platinum coil provides visibility and added safety during Rotational atherectomy.
ASAHI Core Wire Technology
One-piece stainless steel core wire transmits torque for predictable steering.
How it works
Two different wire profiles provide the support you need
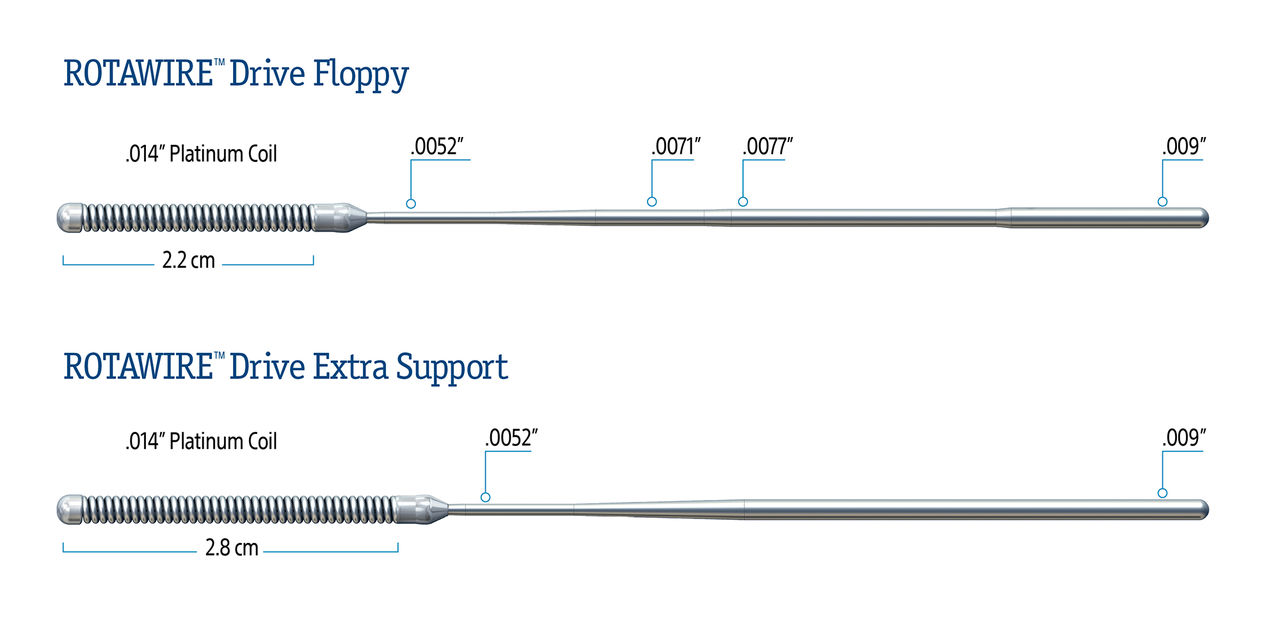
ROTAWIRE Drive Floppy
Floppy is a frontline wire because of its significantly reduced guidewire bias. Its spring tip is 2.2cm.
ROTAWIRE Drive Extra Support
Extra Support is a stiffer frontline wire for distal and heavily calcified proximal lesions with a spring tip of 2.8cm.
- Both wires 330cm total length
- Both wires 0.009” body with 0.014” Spring Tip Diameter
Subscribe for updates on ROTAPRO
Receive timely updates on significant announcements, exclusive opportunities to engage with peers through educational events, and access to valuable tools to enhance your Modern PCI workflow.
Ordering information
ROTAPRO System Console
| Description | Ref/Catalog Number |
|---|---|
| ROTAPRO Console Kit | H749 3930901 0 |
ROTAPRO Pre-Connected Burr and Advancing Device
| Order Number | Description | Burr Size | Length | Maximum Diameter |
|---|---|---|---|---|
| H749 39467125 0 | ROTAPRO Pre-Connected Burr and Advancing Device | 1.25 mm | 135 cm | 0.58 inch |
| H749 39467150 0 | ROTAPRO Pre-Connected Burr and Advancing Device | 1.5 mm | 135 cm | 0.58 inch |
| H749 39467175 0 | ROTAPRO Pre-Connected Burr and Advancing Device | 1.75 mm | 135 cm | 0.58 inch |
| H749 39467200 0 | ROTAPRO Pre-Connected Burr and Advancing Device | 2.0 mm | 135 cm | 0.58 inch |
| H749 39467215 0 | ROTAPRO Pre-Connected Burr and Advancing Device | 2.15 mm | 135 cm | 0.58 inch |
| H749 39467225 0 | ROTAPRO Pre-Connected Burr and Advancing Device | 2.25 mm | 135 cm | 0.58 inch |
| H749 39467238 0 | ROTAPRO Pre-Connected Burr and Advancing Device | 2.38 mm | 135 cm | 0.58 inch |
| H749 39467250 0 | ROTAPRO Pre-Connected Burr and Advancing Device | 2.5 mm | 135 cm | 0.58 inch |
ROTAWIRE™ Drive Guidewire
| Order Number | Description | Length | Tip length | Flexibility | Spring Tip Diameter | Maximum Diameter | Quantity |
|---|---|---|---|---|---|---|---|
| H749 3946300 5 | ROTAWIRE Drive Extra Support Guide Wire with WireClip Torquer | 330 cm | 2.8 cm | Stiff | 0.009 inch | 0.014 inch | Box of 5 |
| H749 3946200 5 | ROTAWIRE Drive Floppy Guide Wire with WireClip Torquer | 330 cm | 2.2 cm | Flexible | 0.009 inch | 0.014 inch | Box of 5 |
Accessories
| Order Number | Description | Quantity |
|---|---|---|
| H802 21600003 1 | Replacement Braided Air Hose | Single |
| H749 3936801 0 | Replacement Power Cord – North America | Single |
| H802 1590101 1 | Regulator Kit – North America | Single |
| H802 22196003 2 | WireClip Torquer | Box of 5 |
ROTAGLIDE™ Lubricant
| Order Number | Description | Quantity |
|---|---|---|
| H7493948300172 | ROTAGLIDE Lubricant Mixture 20 cc vials | Box of 10 |
Subscribe for updates on ROTAPRO
Receive timely updates on significant announcements, exclusive opportunities to engage with peers through educational events, and access to valuable tools to enhance your Modern PCI workflow.
Online medical training and education courses
The EDUCARE online platform makes healthcare education and training more relevant, more comprehensive, more personal, and more accessible. Register to access a library of procedural videos, case studies, training resources, and events.
Subscribe for updates on ROTAPRO
Receive timely updates on significant announcements, exclusive opportunities to engage with peers through educational events, and access to valuable tools to enhance your Modern PCI workflow.
Medicare Inpatient Reimbursement
The U.S. Centers for Medicare & Medicaid Services (CMS) has updated the final inpatient reimbursement for Atherectomy, recognizing the unique procedural role of lesion preparation in PCIs. The information below describes these changes for CMS fiscal year 2026 (FY 2026), effective October 1st 2025. This includes final inpatient DRGs, codes, and payment rates.
Medicare DRGs and Payment Rates for Atherectomy8
Admissions with intraluminal device (with stent placement)
| New Atherectomy DRGs | Abbreviated Description | Finalized 2026 National Average Payment |
|---|---|---|
| 359 | Percutaneous Coronary Atherectomy with Intraluminal Device (Stent) with MCC | $25,022 |
| 360 | Percutaneous Coronary Atherectomy with Intraluminal Device (Stent) without MCC | $17,568 |
Admissions without intraluminal device (without stent placement)
| New Atherectomy DRGs | Abbreviated Description | Finalized 2026 National Average Payment |
|---|---|---|
| 318 | Percutaneous Coronary Atherectomy without Intraluminal Device (Stent) with MCC | $17,626 |
*Percentage change from DRG 251 to DRG 318. The inpatient stay may qualify for additional New Tech Add-on Payment (NTAP), up to $4,013.75, when AGENT™ DCB is used.
Please explore the reimbursement resources below for more information regarding Rotational Atherectomy coding and reimbursement.
For additional questions, please contact the Boston Scientific Reimbursement Support Line: IC.Reimbursement@bsci.com
Additional resources for all sites of service
These resources above are meant to be used by practicing physicians and allied healthcare professionals. These guides are not intended for patients or consumers.
Health economic and reimbursement information provided by Boston Scientific Corporation is gathered from third-party sources and is subject to change without notice as a result of complex and frequently changing laws, regulations, rules, and policies. This information is presented for illustrative purposes only and does not constitute reimbursement or legal advice.
Find additional reimbursement information at the Federal Register: https://www.federalregister.gov/documents/2025/08/04/2025-14681/medicare-program-hospital-inpatient-prospective-payment-systems-for-acute-care-hospitals-ipps-and
1. Allali A, Toelg R, Abdel‐Wahab M, et al. Combined rotational atherectomy and cutting balloon angioplasty prior to drug‐eluting stent implantation in severely calcified coronary lesions: The prepare‐calc‐combo study. Catheterization and Cardiovascular Interventions. 2022;100(6):979-989.
2. Okamoto, Naotaka et al.; presented at Japanese Circulation Society 20232018
3. Okamoto N, Egami Y, Nohara H, et al. Direct comparison of rotational vs orbital atherectomy for calcified lesions guided by optical coherence tomography. JACC: Cardiovascular Interventions. 2023;16(17):2125-2136
4. Bouisset F, Barbato E, Reczuch K, et al. Clinical outcomes of PCI with rotational atherectomy: The European multicentre euro4c registry. EuroIntervention. 2020;16(4). doi:10.4244/eij-d-19-01129
5. Desta L, Jurga J, Völz S, et al. Transradial versus trans-femoral access site in high-speed rotational atherectomy in Sweden. International Journal of Cardiology. 2022;352:45-51
6. Okamoto N, Egami Y, Nohara H, et al. Direct Comparison of Rotational vs Orbital Atherectomy for Calcified Lesions Guided by Optical Coherence Tomography. JACC Cardiovasc Interv. 2023;16(17):2125-2136. doi:10.1016/j.jcin.2023.06.016
7. Allali A, Toelg R, Abdel‐Wahab M, et al. Combined rotational atherectomy and cutting balloon angioplasty prior to drug‐eluting stent implantation in severely calcified coronary lesions: The prepare‐calc‐combo study. Catheterization and Cardiovascular Interventions. 2022;100(6):979-989. doi:10.1002/ccd.30423
8. Data Source: https://www.cms.gov/medicare/payment/prospective-payment-systems/acute-inpatient-pps/fy-2026-ipps-final-rule-home-page#Tables