Boston Scientific accounts are for healthcare professionals only.
PCI complexity is on the rise1
Advancements in technology and operator skill are enabling this minimally invasive approach for more complex coronary artery disease. This trend is reflected in multiple studies, which reveal a significant rise in procedural complexity:
30-35%
Moderate-Severe Calcium2
28-51%
Type C3
10%
ISR (In-Stent Restenosis)4,5
30-67%
Small Vessel6
6%
Nodular7
20%
Long/Diffuse8
20%
Chronic Total Occlusion (CTO)9
15-25%
Bifurcation*,10
5-7%
Left Main (LM)11
Effective interventions require thorough assessment and tailored lesion modification strategies.
*Bifurcations constitute a complex subgroup of lesions characterized by lower procedural success rates and higher rates of adverse outcomes.12
1. Kheifets, M et al. Front Cardiovasc Med. 2022 Jun 24. 2. Généreux, P. et al. J Am Coll Cardiol. 2014 May;63(18):1845-1854. 3. Bortnick A.E. et al. Am J Cardiol. 2014 Feb;113(4):573-9. 4. Tamez H et al EuroIntervention. 2021 Aug;17(5):e380-e387. 5. Moussa ID et al J Am Coll Cardiol. 2020 Sep;76(13):1521-1531. 6. Sanz-Sánchez, J et al. J Struct Cardiov Interv. 2022;1(5):100403. 7. Xu Y et al. Circulation, 2012 Jun; 126(5):537-45. 8. Oh P. et al. Korean Circ J. 2019 Aug;49(8):721-723. 9. Fefer, P et al. J Am Coll Cardiol. 2012 Mar 13;59(11):991-7. 10. Collins, N et al. Am J Cardiol. 2008 Aug 15;102(4):404-10. 11. De Caterina, Alberto R. et al. EuroIntervention. 2013 Mar; 8:1326-1334. 12. Moulias, Athanasios et el. Rev. Cardiovasc. Med. 2023 Mar, 24(3), 8.
Studies confirm the importance of tailoring your device selection strategy
Various clinical scenarios call for distinct preparation methods, emphasizing the need to understand established best practices for the application of each. It is crucial to operate from a versatile toolbox that supports adapting on a case-by-case basis, as over-reliance on any single technology can introduce risks.
ShortCUT: Comparing WOLVERINE™ to IVL* in complex PCI
The ShortCUT trial is the first randomized head-to-head study to compare Cutting Balloon to IVL for the treatment of calcified CAD. The goal of this trial was to compare the efficacy of Cutting Balloon vs. IVL prior to DES implantation in patients with moderate to severely calcified coronary arteries with or without planned atherectomy.
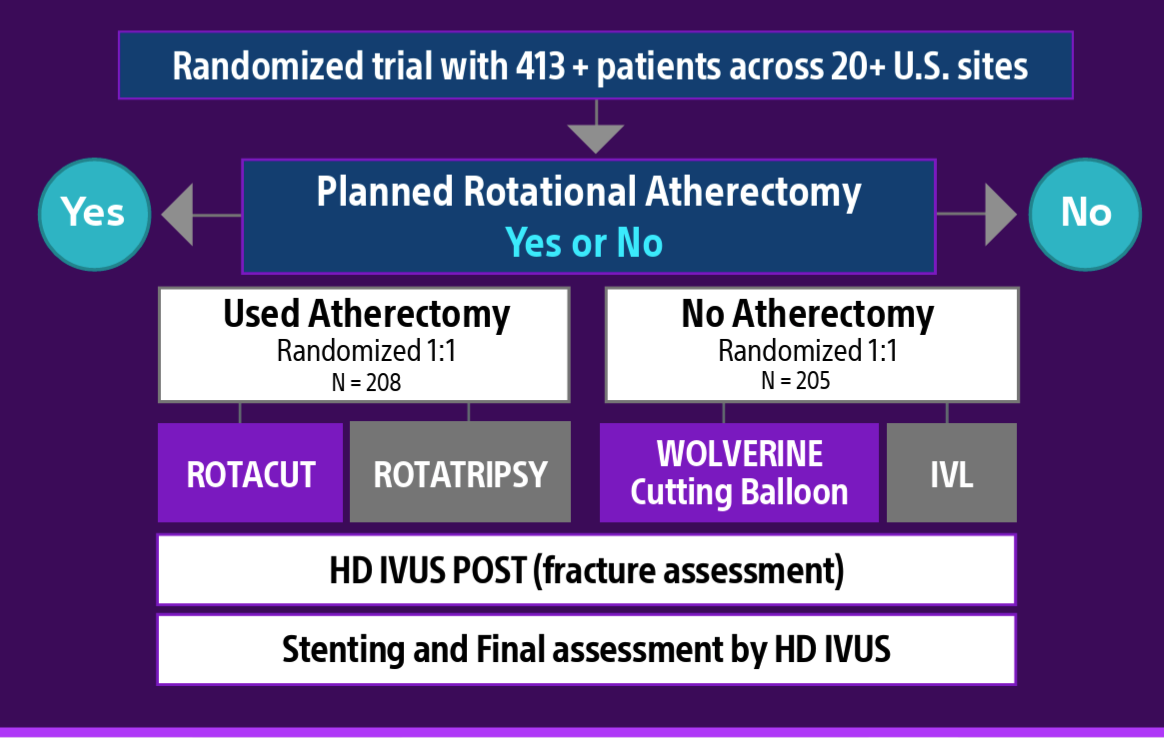
In the ShortCUT trial13, WOLVERINE™ Cutting Balloon™ demonstrated non-inferiority to IVL for minimal stent area (MSA) at the site of maximum calcium in the total study population. There were no statistical differences in stent expansion, presence of calcium fractures, strategy success, intraprocedural adverse events, or MACCE at 30 days between Cutting Balloon and IVL. WOLVERINE also demonstrated total procedural cost savings compared to IVL, primarily driven by the cost of the randomized device.
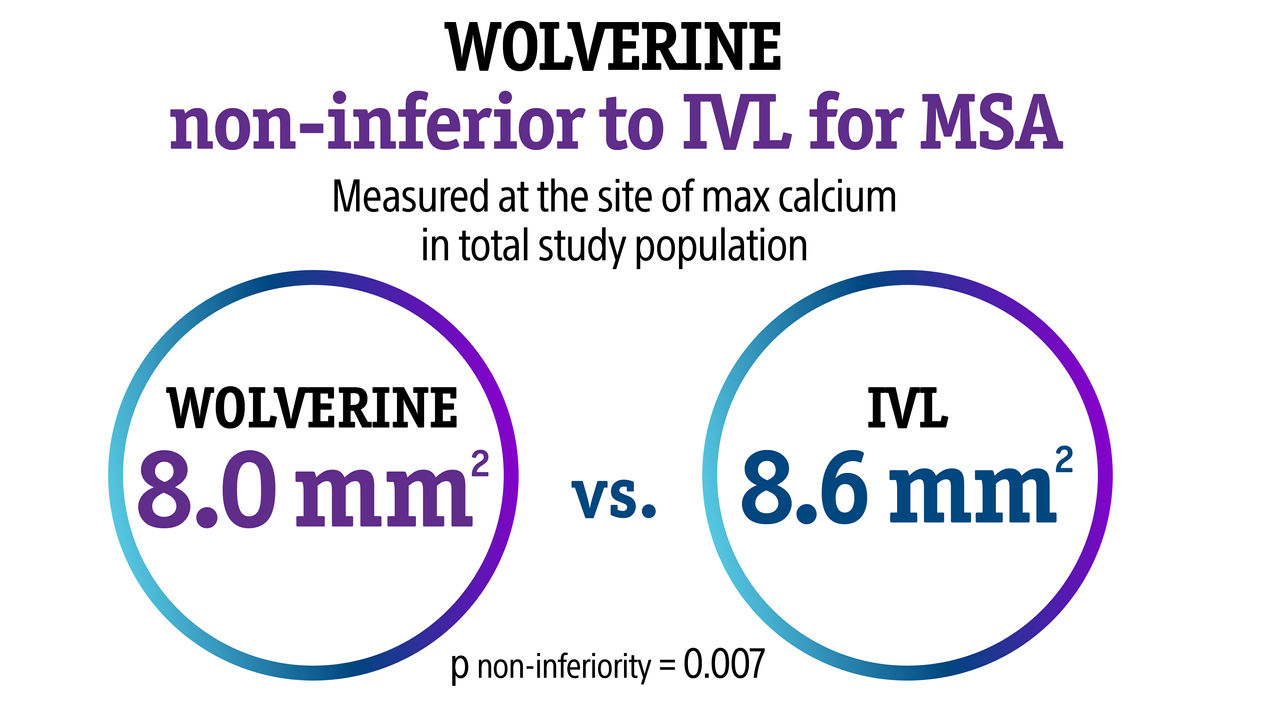
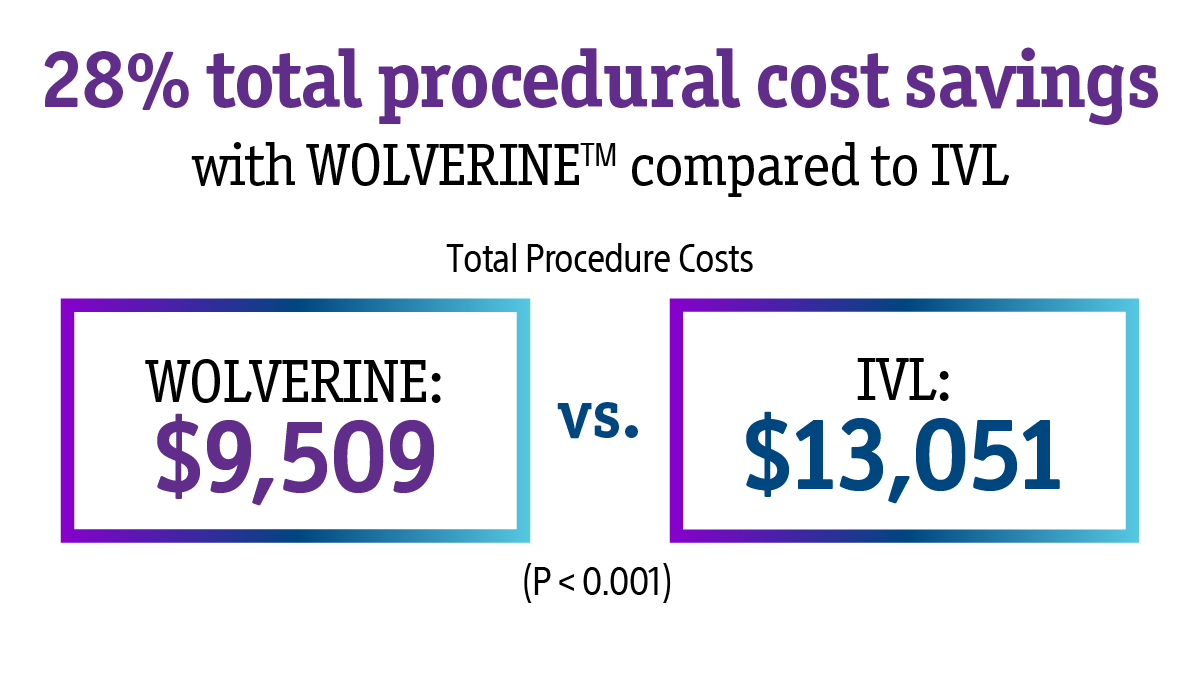
This trial validates the use of WOLVERINE Cutting Balloon as a cost-effective, clinically proven, safe and efficacious option for IVUS-guided treatment of calcified lesions.
13. Data presented at TCT® 2025 by Suzanne Baron, MD.
*Current US market IVL
Rotational atherectomy and cutting balloon combination strategy (ROTACut)
The PREPARE-CALC COMBO14 study found that using the WOLVERINE Cutting Balloon and ROTAPRO™ Rotational Atherectomy System together resulted in significantly higher acute lumen gain in severely calcified lesions compared to using the devices alone.
9 month follow-up
Combination strategy compared to rotational atherectomy or modified balloon alone.
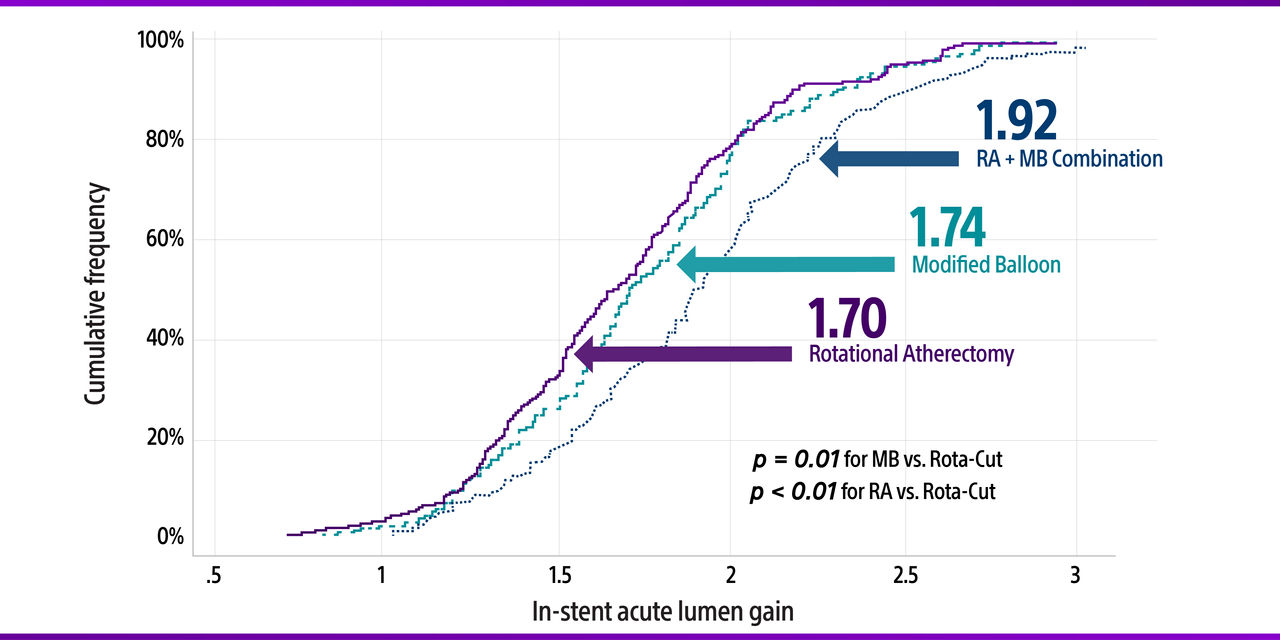
14. Allali A, Toelg R, Abdel-Wahab M, et al. Combined rotational atherectomy and cutting balloon angioplasty prior to drug-eluting stent implantation in severely calcified coronary lesions: The PREPARE-CALC-COMBO study. Catheter Cardiovasc Interv. 2022;100(6):979-989.
Cutting Balloon: safe with maximum impact at lower pressures
Superior calcium lesion prep at lower inflation pressures
In the latest PREDICTION study15, patients treated with Wolverine™ Cutting Balloon demonstrated superior lesion prep treatment measured by greater final MSA at the site of max calcium compared to conventional balloons. (p = 0.0132) The patients had similar characteristics with severely calcific lesions analyzed by IVUS.

To evaluate how the Cutting Balloon enhances lesion preparation in calcified vessels at low atmospheric pressures, physicians compared its use at lower ATM to that of a conventional balloon at higher ATM. The results showed improved lesion modification through cumulative disruption of calcified plaque using the Cutting Balloon at lower pressures.
15. Dr. Kohei Koyama, MD, PhD. A Prospective, Multicenter, Randomized Trial of Cutting Balloon Versus Conventional Balloon for the Treatment of Severe Calcified Lesion (PREDICTION NIRS-IVUS trial). Presented at EuroPCR 2025.
Cutting Balloon vs. POBA
In the COPS Study16, patients were treated with the WOLVERINE™ Cutting Balloon™ or POBA to optimize pre-dilation of calcified lesions before stent implantation. WOLVERINE showed a comparable safety profile to POBA, with no significant differences in procedural complications and one-year MACE. Additionally, WOLVERINE outperformed POBA in achieving greater minimal stent area (MSA) at the calcified segment, with results amplified in the presence of severe calcifications.
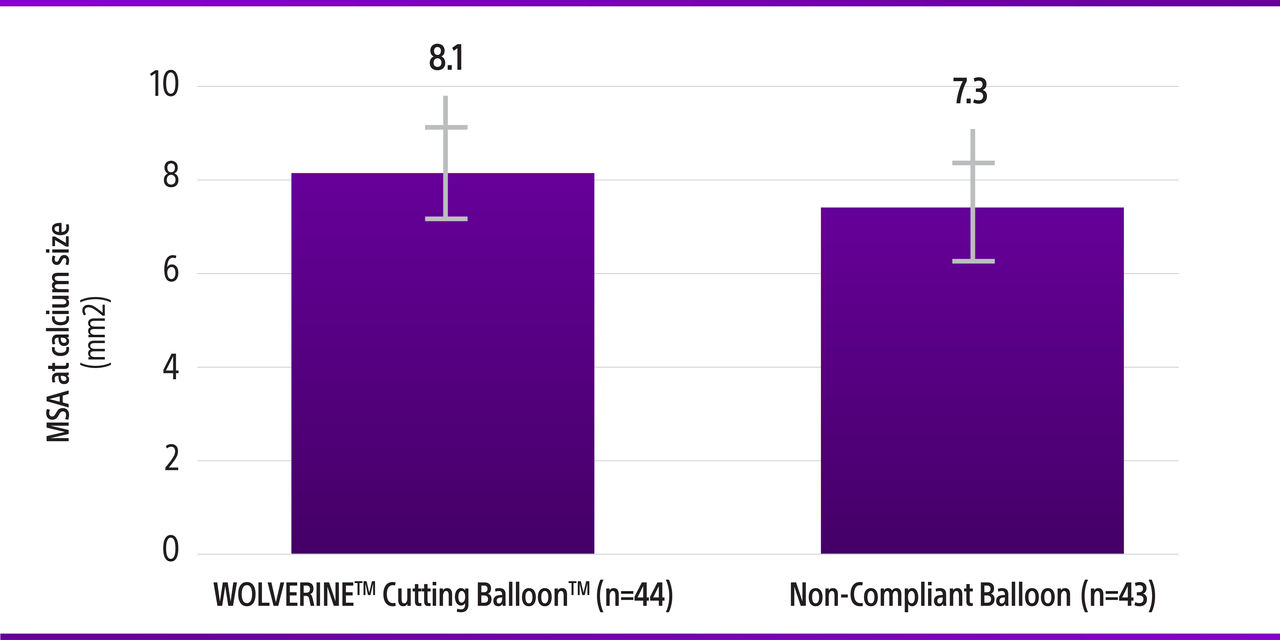
Clinically significant difference in MSA at the calcified segment with WOLVERINE vs. POBA (P = 0.035)
More uniform stent expansion with WOLVERINE vs. POBA. Low rates of procedural complications demonstrated with WOLVERINE.
16. Mangieri, A et al. Cutting balloon to optimize predilation for stent implantation: The COPS randomized trial. Catheter Cardiovasc Interv. 2023 Mar;101(4):798-805.
Cutting Balloon more effective than traditional scoring balloon for plaque modification
The Matsukawa et al Clinical Study17 IVUS and OFDI data suggest that a Cutting Balloon is more effective for plaque modification in cases of severe calcified lesions than traditional scoring balloons. Results were accomplished at lower pressure with WOLVERINE: "This 30% higher lumen gain was achieved with cutting balloon despite using a statistically significant lower inflation pressure than scoring balloon."
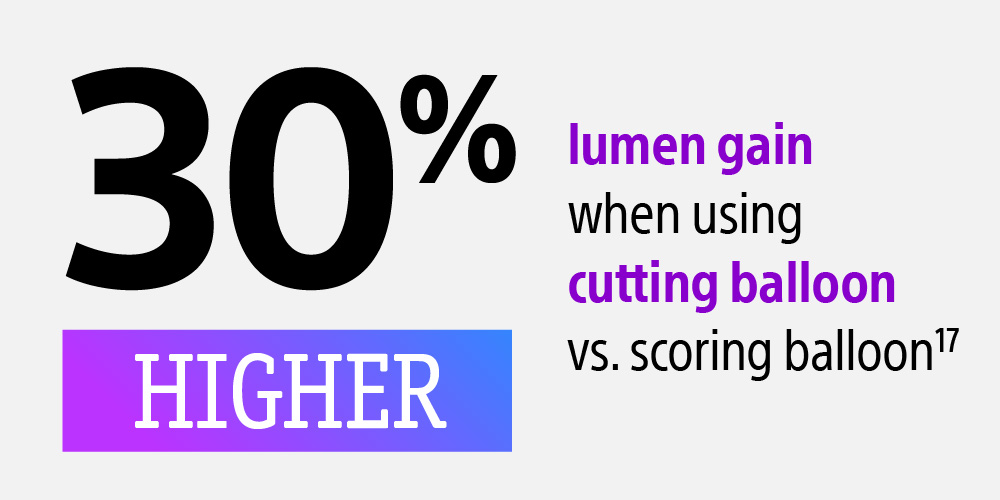
17. Matsukaw a, et al, Cardiovascular Intervention and Therapeutics (2019) 34:325 - 334
Cutting Balloon: Protection from Perforation
The study by Kinnaird et al.18 indicated that Cutting Balloons might be linked to a reduced risk of perforation during PCI procedures. The risk of perforation was significantly lower in cases with Cutting Balloon use (OR 0.62, 95% CI 0.43-0.89, P = 0.01). This extensive analysis, covering over half a million PCI procedures conducted in England and Wales from 2006 to 2013, compared perforation rates in cases with and without the use of Cutting Balloons.
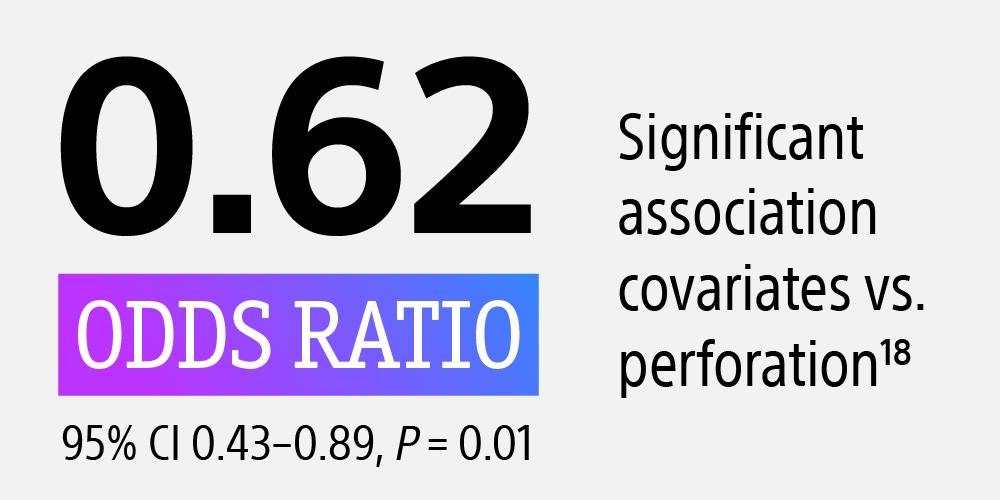
18. Kinnaird T,et al. Circ Cardiovasc Interv. 2016;9(8)
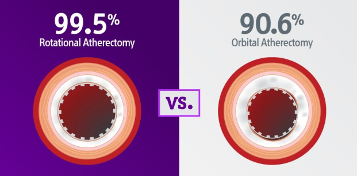
Rotational vs. orbital atherectomy
In the DIRO19 study, greater plaque modification & expansion were shown in patients treated with rotational vs. orbital atherectomy. Additionally, the rotational atherectomy group showed no increased risk – perforations, tamponade, death, and periprocedural MIs were infrequent and comparable.
Plaque Modification (P < 0.01)
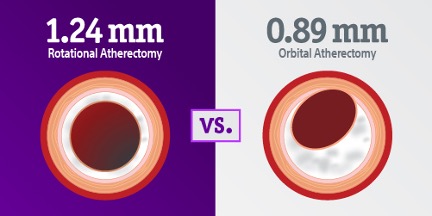
Stent Expansion (P < 0.02)
19. Okamoto N, Egami Y, Nohara H, et al. Direct Comparison of Rotational vs Orbital Atherectomy for Calcified Lesions Guided by Optical Coherence Tomography. JACC Cardiovasc Interv. 2023;16(17):2125-2136. doi:10.1016/j.jcin.2023.06.016

