NC EMERGE™
PTCA Dilatation Catheter
Difference Between Compliant and Non-compliant Balloons During High-pressure Inflation2
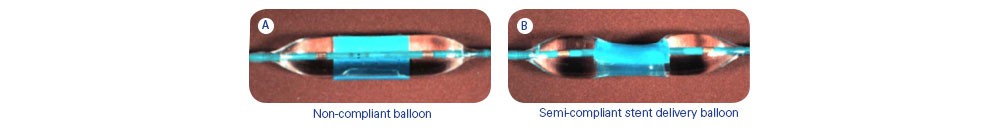
- Semi-compliant balloon demonstrates a “dog-bone” effect at the edge of the cylinder that can damage the vessel wall in vivo
- Incidence of incomplete stent deployment ranges from 20% to 30% of cases
- Adjunctive high-pressure balloon dilation is necessary to improve the minimum stent area and the uniform volumetric stent expansion
Optimizing Stent Deployment Is a Key Element to Obtain Favorable Immediate and
Long-term Results
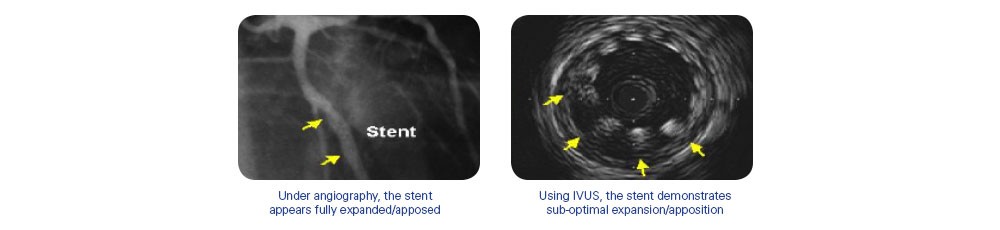
- Incomplete apposition may contribute to thrombosis formation and SATs2,3
- Stent under-expansion may increase risk for restenosis2,7
- Post-dilatation reduces target vessel revascularization (TVR)2,7
- Uniform stent apposition facilitates uniform drug absorption into endothelial tissue3,4,5,6
