Taking your medication
After your procedure, your cardiologist may prescribe medications to thin your blood and prevent blood clots from forming and adhering to the surface of the stent. You should not stop taking these medications unless you are asked to do so by your doctor. If you stop taking these medications before being instructed to do so by your cardiologist, the chances of blood clot formation on the stent, subsequent heart attack, or even death are increased. If surgery or dental work is recommended which would require you to stop taking these medications prematurely, you and your doctor should carefully consider the risks and benefits of this additional surgery or dental work versus the possible risks from early discontinuation of these medications. If you do require premature discontinuation of these medications because of significant bleeding, your cardiologist will carefully monitor you for possible complications. Once your condition has stabilized, your cardiologist will probably put you back on these medications.
Activities and exercises
Your doctor will advise you when it’s safe to resume activities including sports and exercise. Many patients follow their normal routine about a week after stent implantation with the majority of people returning to work only a few days following their procedure.
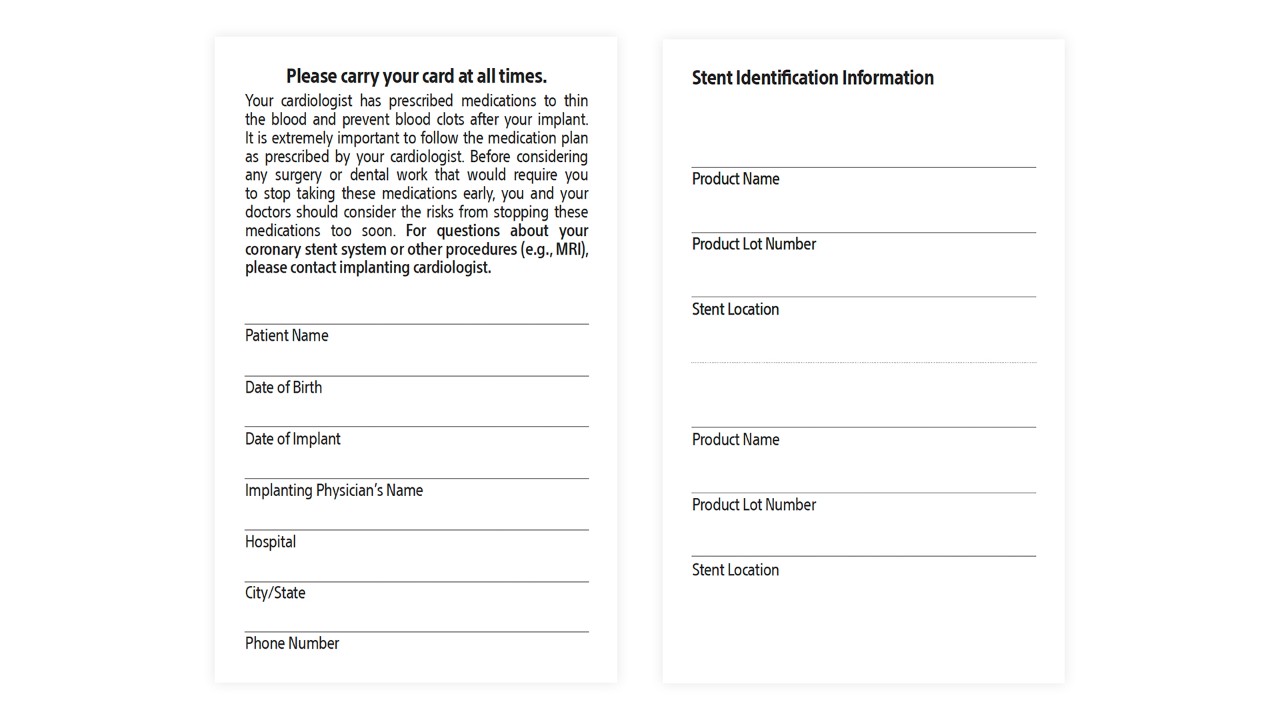
Traveling with your Stent Identification Card
Your stent should not set off medical detector alarms so you can feel confident and safe while traveling. Be sure to carry your Stent Identification Card whether traveling or even running a quick errand. Cards are given at your implant appointment and include your name, your doctor's name and phone number, and the model number of your device and its location. It alerts medical and security personal that you've had a heart procedure.
Replacement cards
If you need a new Stent Identification Card, please reach out to your doctor. You can download and print a copy, or have your doctor send you a new one. Your doctor will need to provide device information for your new stent implant card.
Regular follow-up visits
It’s important to go to all follow-up appointments with your healthcare team, even if you’re feeling well. The first visit is usually two to four weeks after your stent is implanted, with follow-up appointments every six months for the first year. During these visits, your doctor will monitor your progress, evaluate your medications, check the status of your coronary artery disease and determine how the stent is working for you.
When to call a doctor
Your doctor will provide guidelines for when you should contact him or her. But be sure to call your doctor right away if you experience any of the following:
- Chest pain (angina) or more severe or frequent chest discomfort, especially in the first month after your procedure, as these symptoms may indicate a re-narrowing of your coronary arteries
- Shortness of breath
- Sudden weakness or paralysis of the face, arm or leg
- Pain, bleeding or infection at the entry site in your arm or leg
- Any other unexplained symptoms