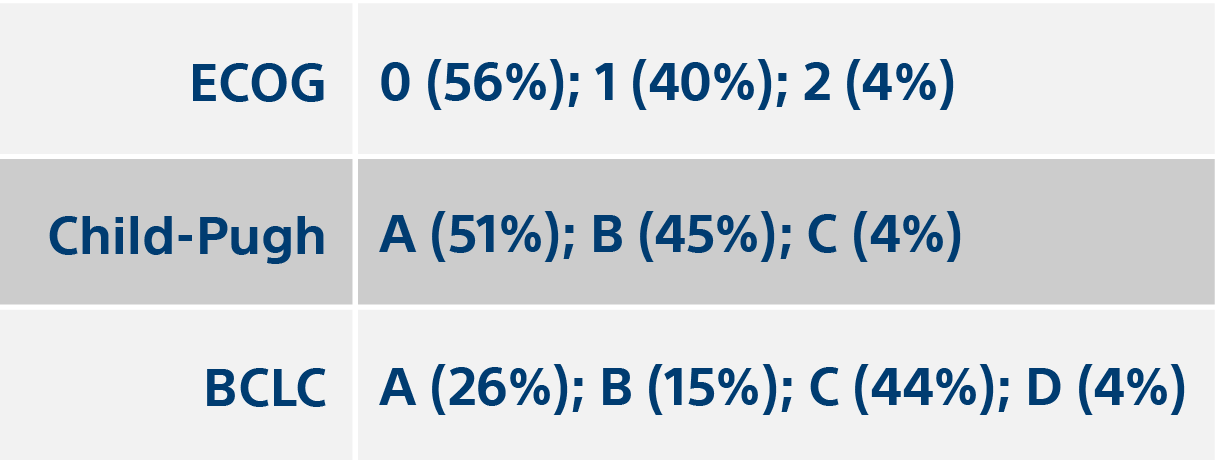
Institutional decision to adopt Y90 as a primary treatment for HCC informed by a 1,000-patient 15-year experience
15 year, 1,000 patient cohort treated with TheraSphere showed benefit vs. standard of care.
Salem R, Gabr A, Riaz A, et al. Institutional decision to adopt Y90 as primary treatment for HCC informed by a 1,000-patient 15-year experience. Hepatology. 2017 Dec 1.

![Table with values for BCLC Stage, Child-Pugh (CP) Score, Median OS [Censored] (months), P-value, Median OS [ITT] (months), P-value.](/en-US/medical-specialties/interventional-radiology/interventional-oncology/therasphere/clinical-data/1000-patient-study/_jcr_content/root/container/container/image_1987547553_cop.coreimg.png/1671049501722/therasphere-1000-patient-bclc-table.png)