Nerve resources
ICE Cryoablation Technology
Key Resources
Explore
Overview
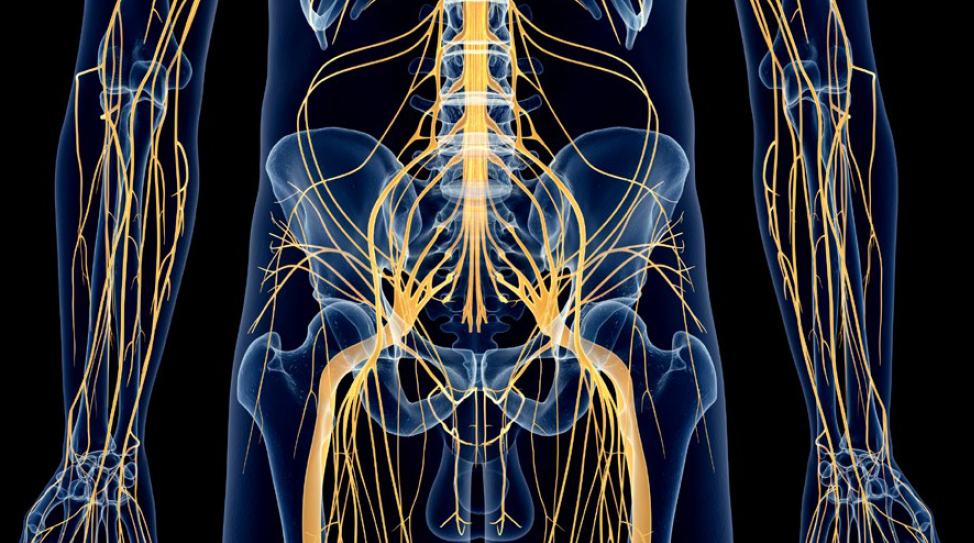
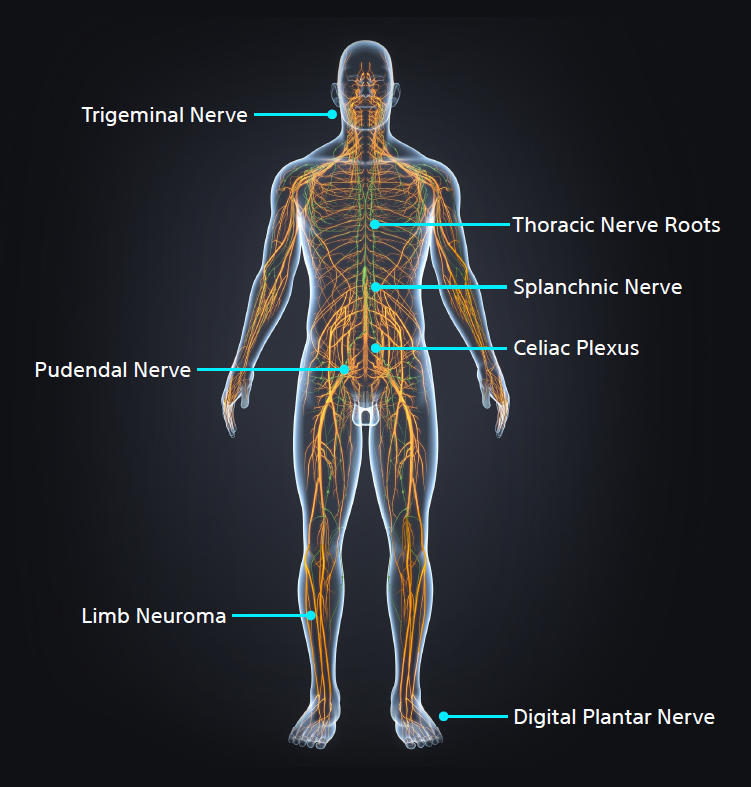
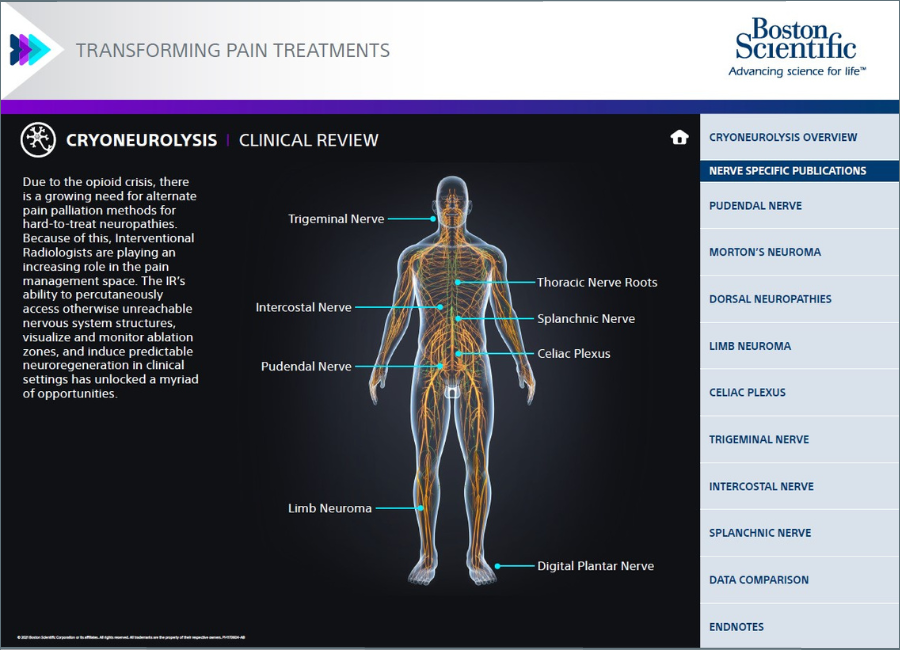
Cryoneurolysis nerve targets
Interventional Radiologists must be aware of key nerve targets, have an in-depth understanding of which patients are candidates for image-guided percutaneous cryoneurolysis (PCA), and the differentiators between cryoablation and heat or alcohol-based neurolysis.
- Pudendal Nerve
- Morton's Neuroma
- Dorsal Neuropathies
- Limb Neuroma
- Celiac Plexus
- Trigeminal Nerve
- Spanchnic Nerve
Case studies
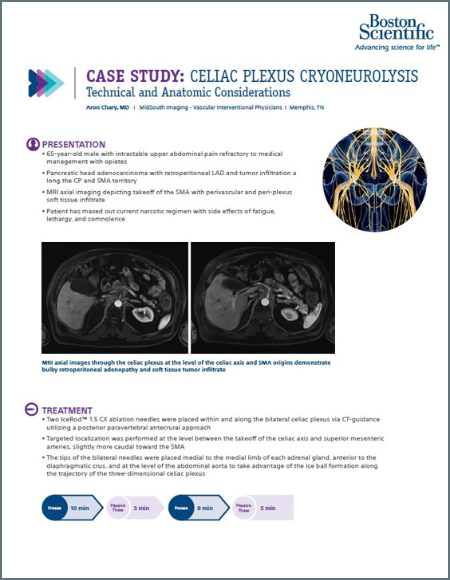
Celiac Plexus Cryoneurolysis: Technical and Anatomic Considerations
A 66-year-old man presented with intractable upper abdominal pain refractory to medical management with opiates. MRI axial images through the celiac plexus at the celiac plexus at the level of the celiac axis and SMA origins demonstrate bulky retroperitoneal adenopathy and soft tissue tumor infiltrate. Two IceRod™ 1.5 CX needles were placed within and along the bilateral celiac plexus via CT-guidance. The CT Axial image (right) in prone position shows right-sided iceball formation along the celiac plexus demonstrating excellent coverage. The patient reported pain at 2/10 after a 3-day follow-up pain assessment; the pain score before the procedure was a 10/10.
Aron Chary, MD I MidSouth Imaging - Vascular Interventional Physicians I Memphis, TN
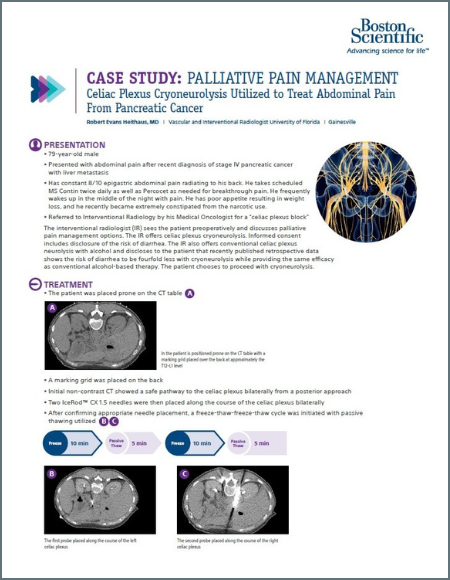
Celiac Plexus Cryoneurolysis Utilized to Treat Abdominal Pain from Pancreatic Caner
A 79-year-old man presented with abdominal pain radiating to his back. He was referred to Interventional Radiology by his Medical Oncologist for a ‘celiac plexus block.’ Two IceRod™ 1.5 CX needles were placed along the course of the celiac plexus bilaterally. The patient experienced mild orthostatic hypotension in the recovery area, a typical transient phenomenon with this treatment. The patient was seen in post-operative clinic one week after the procedure. Pain was down to 3/10 (VAS) from 8/10 (VAS) pre-op with improved appetite, better sleep, and reduced constipation. The pain relief typically last approximately 6-12 months, and the procedure can be repeated should the pain return.
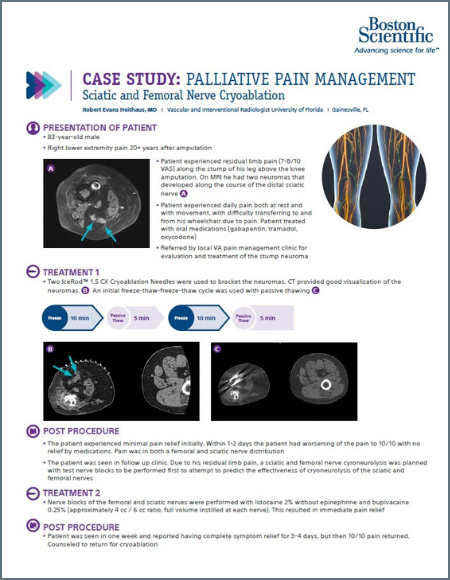
Robert Evans Heithaus, MD I Vascular and Interventional Radiologist University of Florida I Gainesville, FL