Understanding your treatment
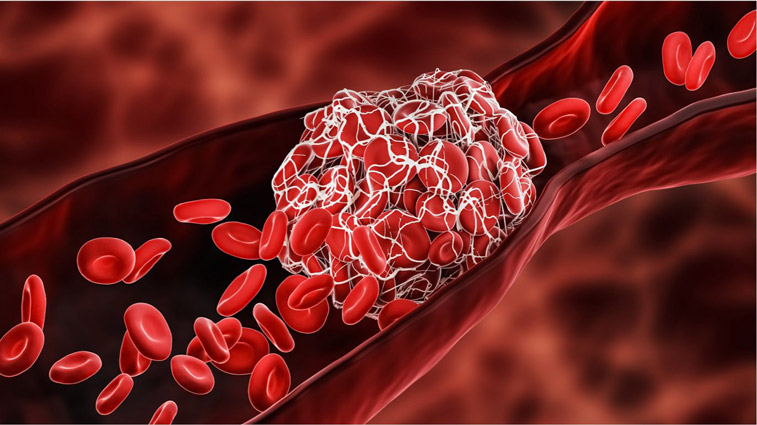
Deep vein thrombosis (DVT) is a large blood clot that forms in one or more of the deep veins in your body. DVT usually happens in the legs or pelvis, but a clot can form anywhere in your body. It’s important to note that approximately 50% of people with DVT experience no symptoms at all.¹
How to spot recurrent DVT
Many DVT blood clots will be absorbed by your body over time with the help of blood thinners. But in the meantime, the clot can cause permanent damage to the valves in your vein, resulting in a condition known as post-thrombotic syndrome (PTS), which causes chronic pain and swelling. Mechanical thrombectomy and IV clot busters may help reduce your risk of developing PTS. The following symptoms may indicate a recurrence of DVT, and you should speak to your doctor.
- Swelling in the affected leg. Rarely, there's swelling in both legs.
- Pain in your leg. The pain often starts in your calf and can feel like cramping or soreness.
- Red or discolored skin on the leg
- A feeling of warmth in the affected leg
Procedures to treat DVT include:
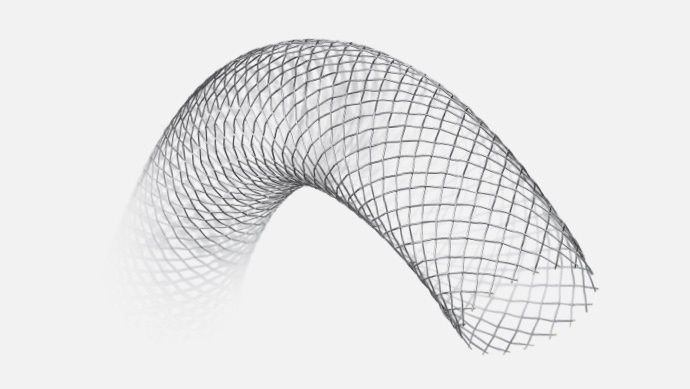
Venous Wallstent™
The Venous Wallstent self-expanding stent is a small, flexible tube specifically designed to hold open the narrowed vein that is partially or completely blocked. The device is collapsed or secured to a long tube called a catheter under a protective sheath or tube. The catheter is then used to deliver the device to the vein where it will be implanted. When the protective sheath is removed, the device expands outward to the walls of the vein. The Venous Wallstent is so flexible, it will mold itself to the vein as it expands.
IV clot buster
IV clot busters, or thrombolytics, are medications placed directly into the clot during a minimally invasive procedure. They’re designed to quickly dissolve clots, restore blood flow, and may help prevent damage to the valves in your vein, which can cause post-thrombotic syndrome.
To administer clot busters, your doctor may sedate you before making a small incision in your groin, wrist, or other location. Your doctor will then use a catheter to deliver medication directly into the clot. Since IV clot busters may cause serious bleeding, they’re usually administered in a hospital or other setting where you can be closely monitored.
Mechanical thrombectomy
Mechanical thrombectomy devices are special catheters designed to help break up and physically remove all or portions of the blood clot during a minimally invasive procedure. A mechanical thrombectomy procedure can help to quickly restore blood flow, reduce medication dosage, and may help prevent damage to the valves in your vein, which can cause post-thrombotic syndrome.
In a mechanical thrombectomy procedure, your doctor may sedate you before making a small incision in your groin, wrist, or other location. The doctor will then insert a specialized tube-like catheter into your veins to access and treat the clot. Your doctor may also deliver IV clot buster medicines during the procedure.
These procedures come with risks and aren’t right for everyone. Be sure to talk to your doctor to find out if they may be right for you.
Knowing your risk
When it comes to DVT, certain things put you in a higher risk category for developing a blood clot. Some are genetic and can’t be changed and others are within your control. Be proactive about your health, and understand your risk factors including:
- A personal or family history of DVT
- Advanced age (risk increases after age 60, but DVT can happen at any age)
- Hormone therapy for birth control or to reduce postmenopausal symptoms
- Pregnancy and the six weeks period following childbirth
- Injury due to surgery, a broken bone, or other trauma
- Prolonged lack of movement due to hospitalization, illness, injury, or paralysis
- Recent or ongoing treatment for cancer, respiratory, or heart failure
- Inflammatory bowel disease, such as ulcerative colitis or Crohn's disease
- Inherited blood disorders that make your blood thicker or more likely to clot
- Varicose veins
- A central venous catheter
- Obesity (body mass index, or BMI, greater than 30kg/m2)
- Smoking
Healthy living after your procedure
Do your part to reduce your risk of DVT after your procedure. The following lifestyle changes can help protect you from blood clots:
- Wear compression stockings when traveling by air
- Get up and walk as frequently as possible on overseas flights
- Schedule walking breaks and do leg exercises to keep blood flowing when sitting for long periods of time.
- Stop smoking and commit to a healthy lifestyle
Stent Implant Card
Whether you’re running a quick errand or going on vacation, it’s important to carry your Stent Implant Card with you at all times. If you receive dental or medical care or report to an emergency room, show your Stent Implant Card. You will be given your card at the time of your procedure. Your implant card contains your name, your doctor’s name and phone number, and information about your implanted stent(s).
Regular follow-up visits
It’s important to maintain all follow-up visits, even if you’re feeling well. During these visits, your doctor will monitor your progress, evaluate your medications and check the status of your overall health to determine the success of your procedure.