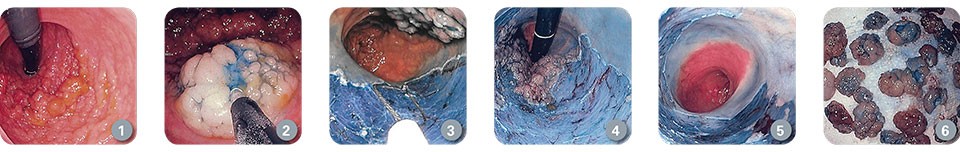
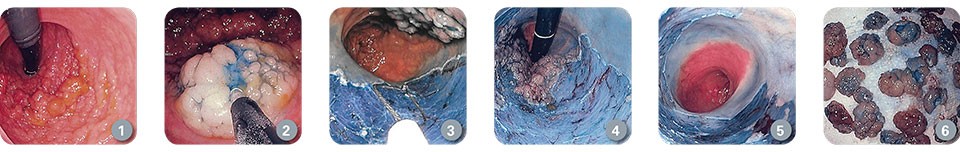
Technique Spotlight: Tubulovillous Adenoma with Intramucosal Adenocarcinoma

Patient History
Procedure
Boston Scientific accounts are for healthcare professionals only.
Create an account to access online training and education on EDUCARE, manage your customer profile, and connect with customer support and service teams.
My Boston Scientific account
Access your online applications and manage your customer profile.
Quick Links
Call customer care