Our extensive stent portfolio provides functionality and flexibility
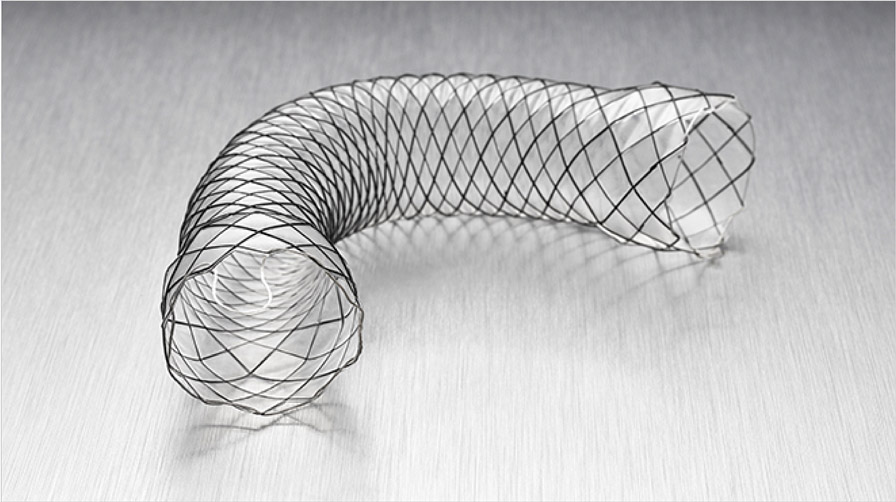
Agile™ Esophageal Stent System
Offers a flexible and conformable self-expanding metal stent on a through the scope delivery system which enables direct visualization during deployment and may help minimize reliance on fluoroscopy.
WallFlex™ Esophageal Stent
Delivers luminal patency in patients with esophageal strictures caused by intrinsic and/or extrinsic malignant tumors, through a combination of flexibility and control for optimized patient care.
Ultraflex™ Esophageal Stents
There is a covered and an uncovered Ultraflex stent. These stents are designed to maintain luminal patency in esophageal strictures caused by intrinsic and/or extrinsic malignant tumors.
Recovering from your procedure
Your esophageal stent procedure will likely be performed on an outpatient basis. After your procedure, you will rest and recover as your care team monitors your progress for a few hours. As you are ready, the doctor will release you to go home. Make sure someone is there to drive you as you will still be unsteady from the anesthesia. Discomfort immediately following your procedure is normal. Your doctor may prescribe you over-the-counter pain medicines as you need them.¹
Eating with your stent
Once the stent has been placed, your medical team will advise you on when it is safe to start eating and drinking again. You will start with fluids and then build up gradually to a soft diet. Depending on your type of stent, it can typically take one to two days for the stent to fully expand, so take it slow at first and eat small meals made up of soft foods.
Foods to avoid
The stent has been placed to allow you to eat as normally as possible. However, it is possible for the stent to become blocked. The most common reason for blockage is from food that is swallowed without being sufficiently chewed or from foods that do not break down enough when chewed. The following foods can be difficult to break down, despite chewing, and so are more likely to cause your stent to become blocked:
Bread and toast
Tough and gristly meat
Hard boiled or fried egg
Fish with bones
Oranges, grapes and pineapple
Stringy vegetables (e.g., greenbeans, celery)
Potato skins
Salad items (e.g., salad leaves and lettuce)
Raw vegetables
Chips
Ice cream or yogurt with chunks of fruit, cereal or nuts
Tips for eating with your stent
Take your time, and eat slowly
Eat small meals. Aim for 5 to 6 small meals a day rather than 3 large meals
Cut your food into small pieces, take small bites, and chew thoroughly
Use sauces, gravy, and cream to add moisture to your meals. This will help food pass through your stent
Drink throughout your meal to help clear your stent. Warm or carbonated beverages are recommended, but all fluids are beneficial. For some people, carbonation may worsen symptoms of heartburn or acid reflux
Sit up straight as you are eating and for a few hours afterwards
If you take pills, ask your doctor if they are available in liquid form
What to do if you feel your stent is blocked
Do not panic. The blockage only affects the tube in your stomach and not your ability to breathe
Stop eating, stand up, and take a few sips of water
Try a carbonated beverage
Walk around
If the stent blockage has not cleared after one or two hours, contact your doctor or nurse
When to call your doctor
Call your doctor immediately if you experience the following:
Fever
Sever acid (gastroesophageal) reflux
Persistent swallowing problems
Pain that persists longer than 72 hours or is severe
Regular follow-up visits
It’s important to maintain all follow-up visits, even if you’re feeling well. During these visits, your doctor will monitor your progress, evaluate your medications, check the status of your overall health and determine the success of your stent procedure.
Magnetic Resonance (MR) Conditional
Non-clinical testing has demonstrated that the WallFlex Esophageal Stent System, Ultraflex Esophageal NG Stent System and Agile Esophageal Stent System are MR Conditional. These stents can be scanned safely under the conditions outlined in each device Instructions for Use.
Please consult with your physician. Your physician should refer to the package insert for details. Prescriptive information for each device can be found here.
Download the Ultraflex Esophageal NG Stent System