Pulmonology / Technique Spotlight with Sandra Ettema, MD
Technique Spotlight with Sandra Ettema, MD
54-year-old female with history of gallbladder removal which required intubation for a short period of time in 2012. Following the intubation, the patient experienced stridor and difficulty breathing. The physician performed a bronchoscopy and CO2 laser excision with balloon dilation of tracheal stenosis. She went 4 years until she saw a community physician in 2016 who underwent the same procedure as in 2012 and applied Mitomycin-C. Since her surgery in 2016, she has been on acid reflux medication.
Patient was referred to our practice by local ENT in January 2018 due to worsening tightness with breathing and stridor at rest. The patient did not report any upper respiratory tract illnesses within the last year as well as no increase in acid reflux symptoms. She did report clinical symptoms including difficulty breathing while walking across the room and significant increase of symptoms after climbing a single flight of stairs. The patient is slightly overweight and is a lifelong non-smoker. We performed an in-office bronchoscopy and found significant stenosis (Figure 1). We were also able to attain a 3-D CT noting extent of stenosis (Figure 2).
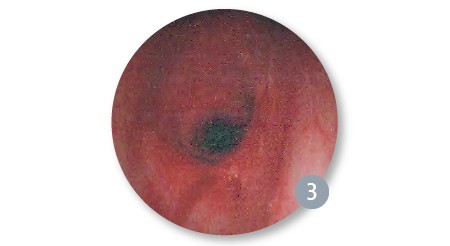
A 3.5 bronchoscope and a tracheostomy surgical set up was prepared at the back table in case of emergency as her airway was measured on CT as 5mm transversely and 12 mm in the AP direction. We were able to bag mask ventilate the patient without difficulty and a Dedo laryngoscope was placed. The patient’s glottis was difficult to visualize. The larynx was anteriorly displaced. After multiple laryngoscopes were attempted, the wide anterior commissure scope from the Steiner set was placed successfully with wide tape across the external neck of the patient. We then used the 4-0 cuffless micro-laryngoscopy tube to intubate the patient through the laryngoscope which established the airway. Once the airway was established, we could directly visualize the stenosis and airway with a 0-degree telescope (Figure 3).
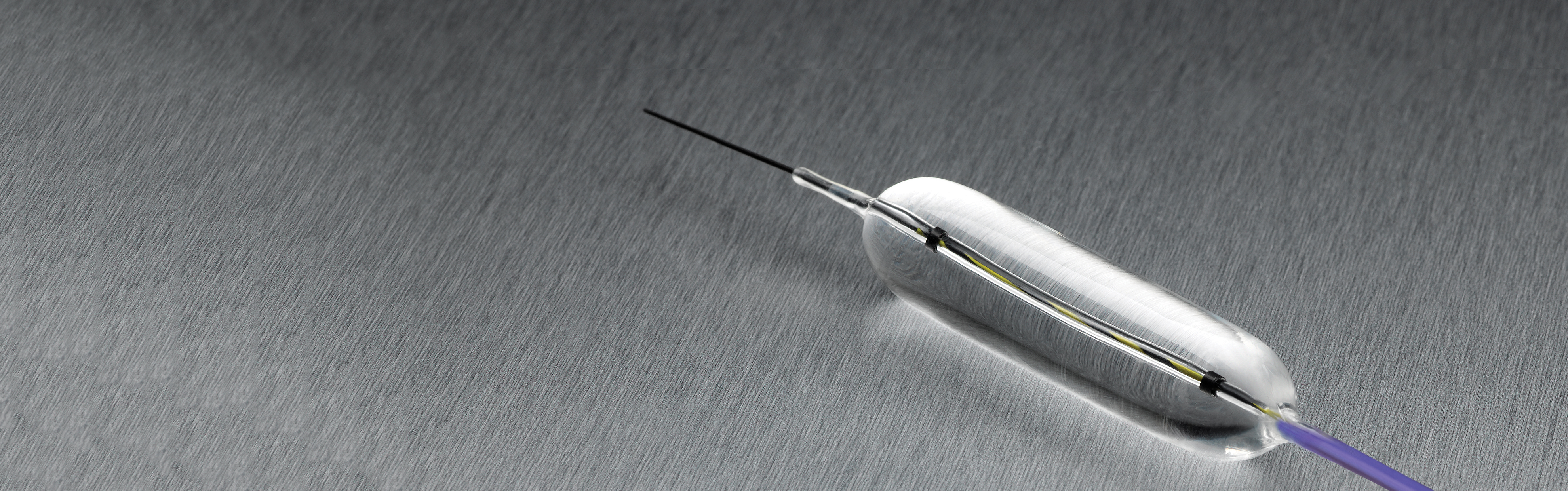
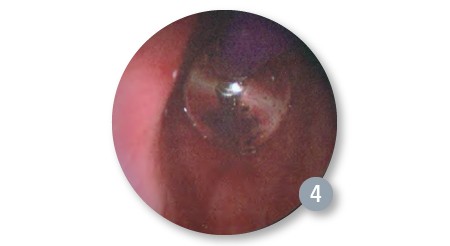
We proceeded with serial balloon dilation first using the CRE™ Pulmonary Balloon Dilatation Catheter (CRE Pulmonary Balloon) sized 8/9/10mm, which after successful use provided a larger airway to place a 5.5 uncuffed endotracheal tube to allow for better ventilation between dilations. We then proceeded with the following sized balloons: 10/11/12mm, 12/13.5/15mm, 15/16.5/18mm, and 18/19/20mm balloons alternating endotracheal tubes up to 6.5 cuffed into the airway for adequate ventilation. Serial dilation was completed after 19mm.
Pre-Dilation (Operating Room)
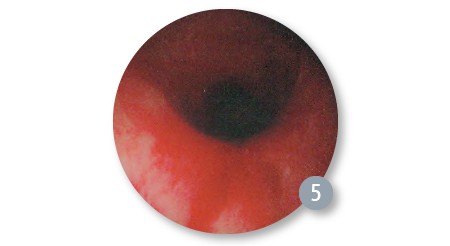
Post 1st Dilation with 8/9/10mm Balloon
Size 8/9/10mm Balloon Expanded
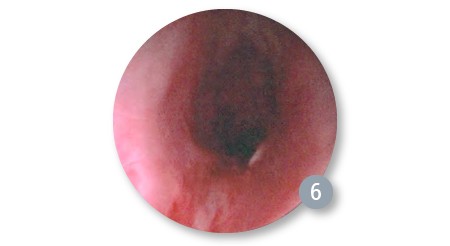
Post Final Dilation (Used 18/19/20mm balloon and was complete after 19mm)
Discussion/Conclusions/Recommendations
Utilizing the CRE Pulmonary Balloons enabled us to use less instrument manipulationbecause the balloon was able to dilate the stricture extremely effectively and in atraumaticfashion, potentially giving the patient a better outcome. We were able to perform serialballoon dilations utilizing multiple balloons in which each balloon performed excellently.I would recommend the CRE Pulmonary Balloons to my peers as a surgical tool to aid invisualizing the airway in any patient with airway stenosis.