Boston Scientific accounts are for healthcare professionals only.
BVN ablation treatment in multiple studies: Mean visual analog scale (VAS) over time 2, 3, 6-9
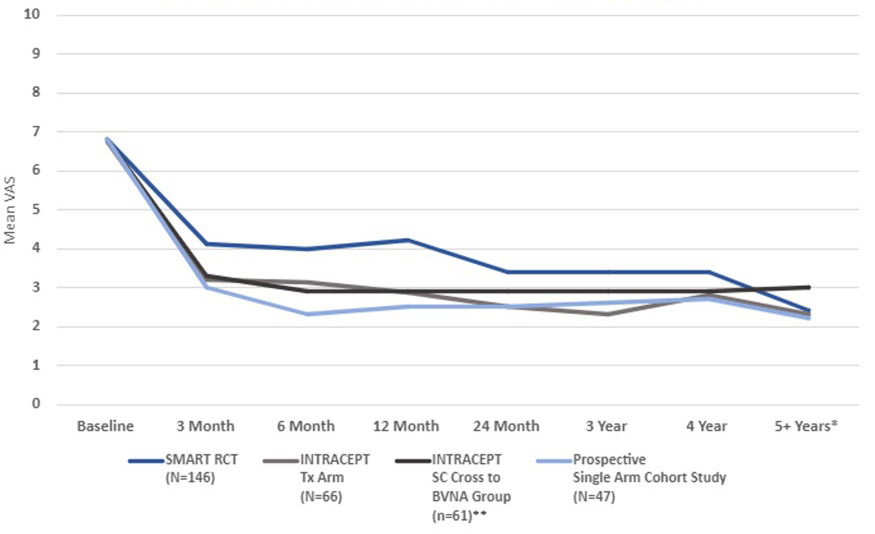
*SMART RCT US per protocol treatment arm at mean of 6.4 years
** Standard arm re-baselined and offered active treatment of a median of 5.8 months
†p-value from paired t-tests for BVN ablation arm patients with a 5-year visit
Mean VAS over time
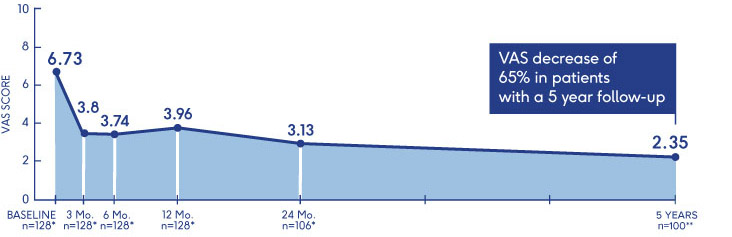
*n=Global PP **n=US PP
*p-value from paired t-tests for BVN ablation arm patients with a 5-year visit
†p-values from paired t-tests of BVN ablation arm patients with a 24-month visit
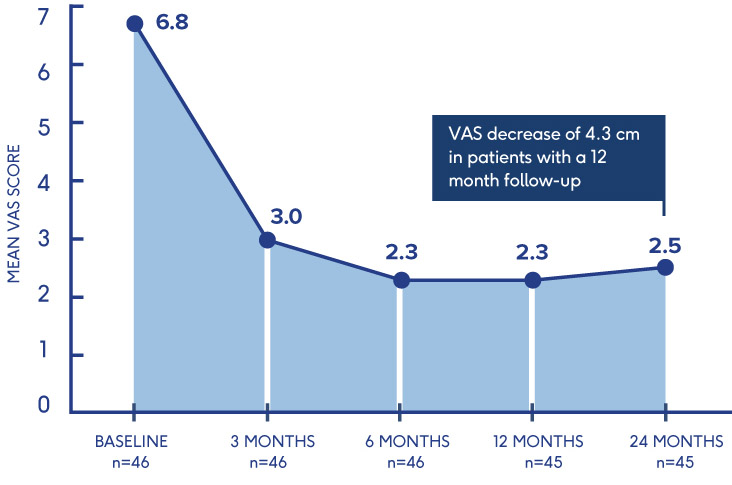
Mean VAS: baseline to 24 months
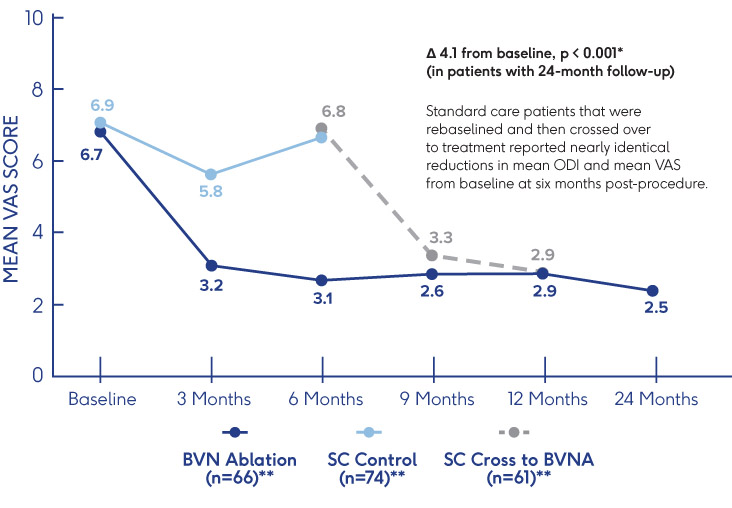
*p-value from a t-test on the basivertebral nerve ablation treatment arm with a 24-month visit.
**Multiple imputations for 3 Month ODI missing values. All other measurements as observed, no imputations for missing data.
†p-values from paired t-tests of BVN ablation treated patients with a 12-month visit
Mean VAS over time
(Baseline to 12 months, p<0.001)
*p-values from paired t-tests of BVN ablation treated patients with a 12-month visit.
Looking for more proof?
Becker S, Hadjipavlou A, Heggeness M, Ablation of the basivertebral nerve for treatment of back pain: a clinical study. The Spine Journal: Official Journal of the North American Spine Society 2017; 17: 218-223
Fischgrund JS, Rhyne A, Franke J, et al. Intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. 2018;27(5):1146-56. doi: 10.1007/s00586-018-5496-1
Fischgrund JS, Rhyne A, Franke J, et al. Intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 2-year results from a prospective randomized double-blind sham-controlled multicenter study. Int J Spine Surg. 2019;13(2):110-9.doi:10.14444/6015
Fischgrund J, Rhyne A, Macadaeg K, et al. Long-term outcomes following intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 5-year treatment arm results from a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. 2020;29(8):1925-34.doi.org/10.1007/s00586-020-06448-x
Khalil, J., et al. Intraosseous basivertebral nerve ablation: 5-year outcomes from three long-term follow-up studies.
Interventional Pain Medicine, Volume 3, Issue 4, 2024,100529, ISSN 2772-5944, https://doi.org/10.1016/jinpm.2024.100529
Khalil J. Pooled Intraosseous Basivertebral Nerve Ablation: 4-Year Effectiveness and Safety Results from Two Long-Term Follow-up Studies. Lecture ASPN annual meeting; July 13-16, 2023. Miami, FL.
Khalil JG, Smuck M, Koreckij T, et al. A prospective, randomized, multicenter study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain. Spine J. 2019;19(10):1620-32. doi:10.1016/j spinee.2019.05.598
Koreckij T, Kreiner S, Khalil JG, Smuck M, Markman J, Garfin S. Prospective, randomized, multicenter study of intraosseous basivertebral nerve ablation for thetreatment of chronic low back pain: 24-month treatment arm results. NASS). Published online October 26, 2021. DOI: https://doi.org/10.1016/j.xnsj.2021.100089
Macadaeg K, Truumees E, Boody B, Pena E, Arbuckle A., Gentile, J, et al. A prospective, open-label, single-arm, multi-center study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 12-month results. NASS) 2020;3(100030). E-pub 18 Sept 2020. https://doi.org/10.1016/j.xnsj.2020.100030
Markman JD, Rhyne A, Sasso R, et al. Association between opioid use and patient-reported outcomes in a randomized trial evaluating basivertebral nerve ablation for the relief of chronic low back pain. Neurosurgery: March 2020 – Volume 86 – Issue 3 – p 343-347 doi: 10.1093/neuros/nyz093
Smuck M, Khalil JG, Barrett K, Hirsch JA, Kreiner S, Koreckij T, et al. Prospective, randomized, multicenter study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 12-month results. Reg Anesth Pain Med. 2021;0:1-5. doi:10.1136/rapm-2020-102259
Smuck M, Truumees E, Macadaeg K, Jaini AM, Chatterjee S, Levin J. Intraosseous basivertebral nerve ablation: pooled long-term outcomes from two prospective clinical trials. Interventional Pain Medicine. 2023; 2(2). https://doi.org/10.1016/j.inpm.2023.100256.
Truumees E, Macadaeg K, Pena E, Arbuckle A, Gentile, J, Funk R, et al. A prospective, open-label, single-arm, multi-center study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain. ESJ 2019;28:1594-1602. https://doi.org/10.1007/s00586-019-05995-2
Conger A, Burnham TR, Clark T, Teramoto M, McCormick ZL. The Effectiveness of Intraosseous Basivertebral Nerve Radiofrequency Ablation for the Treatment of Vertebrogenic Low Back Pain: An Updated Systematic Review with Single-Arm Meta-analysis. Pain Medicine. 2022;23(Suppl_2):S50-S62. https://doi.org/10.1093/pm/pnac070
Conger A, Schuster NM, Cheng DS, Sperry BP, Joshi AB, Haring RS, Duszynski B, McCormick ZL. The Effectiveness of Intraosseous Basivertebral Nerve Radiofrequency Neurotomy for the Treatment of Chronic Low Back Pain in Patients with Modic Changes: A Systematic Review. Pain Medicine. 2021;22(5):1039-1054. https://doi.org/10.1093/pm/pnab040
Michalik A, Conger A, Smuck M, Maus TP, McCormick ZL. Intraosseous Basivertebral Nerve Radiofrequency Ablation for the Treatment of Vertebral Body Endplate Low Back Pain: Current Evidence and Future Directions. Pain Medicine. 2021;22(Supp|_1):524-530. https://doi.org/10.1093/pm/pnab117
Schnapp W, Martiatu K, Delcroix G. Basivertebral Nerve Ablation for the Treatment of Chronic Low Back Pain: A Scoping Review of the Literature. Pain Physician. 2022:E551-E562.
Tieppo Francio V, Sherwood D, Twohey E, Barndt B, Pagan-Rasodo R, Eubanks J, Sayed D. Developments in Minimally Invasive Surgical Options for Vertebral Pain: Basivertebral Nerve Ablation – A Narrative Review. J Pain Res.
2021;14:1887-1907.
Urits I, Noor N, Johal AS, Leider J, Brinkman J, Fackler N, Vij N, An D, Cornett EM, Kaye AD, Viswanath O. Basivertebral Nerve Ablation for the Treatment of Vertebrogenic Pain. Pain Ther. 2021;10(1):39-53. https://doi.org/10.1007/s40122-020-00211-2
Lorio M, Clerk-Lamalice O, Beall D, Julien T. International Society for the Advancement of Spine Surgery Guideline-Intraosseous Ablation of the Basivertebral Nerve for the Relief of Chronic Low Back Pain. Int J Spine Surg. 2020;14(1):18-25. https://doi.org/10.14444/7002
Sayed D, Grider J, Strand N, et al. The American Society of Pain and Neuroscience (ASPN) Evidence-Based Clinical Guideline of Interventional Treatments for Low Back Pain. J Pain Res. 2022;15:3729-3832.
https://doi.org/10.2147/JPR.S386879
Sayed D, Naidu RK, Patel KV, et al. Best Practice Guidelines on the Diagnosis and Treatment of Vertebrogenic Pain with Basivertebral Nerve Ablation from the American Society of Pain and Neuroscience. J Pain Res. 2022;15:2801-2819. https://doi.org/10.2147/JPR.S378544
Boody B, Sperry BP, Harper K, Macadaeg K, McCormick ZL. The Relationship Between Patient Demographic and Clinical Characteristics and Successful Treatment Outcomes After Basivertebral Nerve Radiofrequency Ablation: A Pooled Cohort Study of Three Prospective Clinical Trials. Pain Medicine. 2022;23(Suppl_2):S2–S13. https://doi.org/10.1093/pm/pnac050
Conger A, Smuck M, Truumees E, Lotz JC, et al. Vertebrogenic Pain: A Paradigm Shift in Diagnosis and Treatment of Axial Low Back Pain. Pain Medicine. 2022;23(Suppl_2):S63–S71. https://doi.org/10.1093/pm/pnac081
McCormick Z, Sperry BP, Boody BS, et al. Pain Location and Exacerbating Activities Associated with Treatment Success Following Basivertebral Nerve Ablation: An Aggregated Cohort Study of Multicenter Prospective Clinical Trial Data. Pain Medicine. 2022;23(Suppl_2):S14–S33. https://doi.org/10.1093/pm/pnac069
McCormick ZL, Conger A, Smuck M, et al. Magnetic Resonance Imaging Characteristics Associated with Treatment Success from Basivertebral Nerve Ablation: An Aggregated Cohort Study of Multicenter Prospective Clinical Trials Data. Pain Medicine. 2022;23(Suppl_2):S34–S49. https://doi.org/10.1093/pm/pnac093
Schnapp W, Schnapp M, Gottlieb J, Alexandre LC, Martiatu K, Delcroix G. Prospective Cohort Study of Basivertebral Nerve Ablation for Chronic Low Back Pain in a Real-World Setting: 12-Month Follow-Up. Interventional Pain Medicine. 2024;3(4):100446. https://doi.org/10.1016/j.inpm.2024.100446
Kreiner S, Reiter MF, Bydon M, Schneider BJ, et al. Basivertebral Nerve Ablation, Defining Appropriate Coverage Positions. North American Spine Society. Published February 2023. ISBN 978-1-929988-77-X
McCormick Z, Curtis T, Cooper A, Wheatley M, Smuck M. Low Back Pain-related Healthcare Utilization following Intraosseous Basivertebral Nerve Radiofrequency Ablation: A Pooled Analysis from Three Prospective Clinical Trials, Pain Medicine, 2023:, pnad114, https://doi.org/10.1093/pm/pnad114
Smuck M, McCormick ZL, Gilligan C, et al. A Cost-Effectiveness Analysis of Intraosseous Basivertebral Nerve Ablation for the Treatment of Chronic Low Back Pain. The Spine Journal. Published online September 25, 2024. https://doi.org/10.1016/j.spinee.2024.09.016
Data on file.
- Fischgrund J, Rhyne A, Macadaeg K, et al. Long-term outcomes following intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 5-year treatment arm results from a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. 2020;29(8):1925-34. doi.org/10.1007/s00586-020-06448-x
- Koreckij T, Kreiner S, Khalil G, Smuck M, Markman), GarfinS. Prospective, randomized, multicenter study of intraosseous basivertebral nerve ablation for the
treatment of chronic low back pain: 24-month treatment arm results. NASS]. Published online October 26, 2021. DOI:
https://doi.org/10.1016/j.xnsj.2021.100089 - Fischgrund JS, Rhyne A, Franke J, et al. Intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. 2018;27(5):1146-56. doi:10.1007/s00586-
018-5496 - Fischgrund JS, Rhyne A, Franke J, et al. Intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 2-year results from a prospective randomized double-blind sham-controlled multicenter study. Int Spine Surg. 2019;13(2):110-9.
doi:10.14444/6015 - K. Macadaeg, E. Truumees, B. Boody, E. Pena, J. Arbuckle II, J. Gentile, R. Funk, D. Singh, S. Vinayek, A prospective, single arm study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 12-month results, North American Spine Society Journal (NASS]) (2020), doi.org/10.1016/j.xnsj.2020.1
- Smuck M, Khalil JG, Barrett K, Hirsch JA, Kreiner S, KoreckiT, et al. A prospective, randomized, multi-center study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 12-month results. Reg Anesth Pain Med. 2021;rapm-
2020-102259. doi:10.1136/rapm-2020-102259 - Khalil, J., et al. Intraosseous basivertebral nerve ablation: 5-year outcomes from three long-term follow-up studies. Interventional Pain Medicine, Volume 3, Issue 4, 2024,100529, ISSN 2772-5944, https://doi.org/10.1016/j.inpm.2024.100529.
- Smuck M, Truumees E, Macadaeg K, Jaini AM, Chatterjee S, Levin J. Intraosseous basivertebral nerve ablation: pooled longterm outcomes from two prospective clinical trials. Interventional Pain Medicine. 2023; 2(2).
https://doi.org/10.1016/j.inpm.2023.100256. - Becker S, Hadjipavlou A, Heggeness M, Ablation of the basivertebral nerve for treatment of back pain: a clinical study. The Spine Journal: Official Journal of the North American Spine Society 2017; 17: 218-223