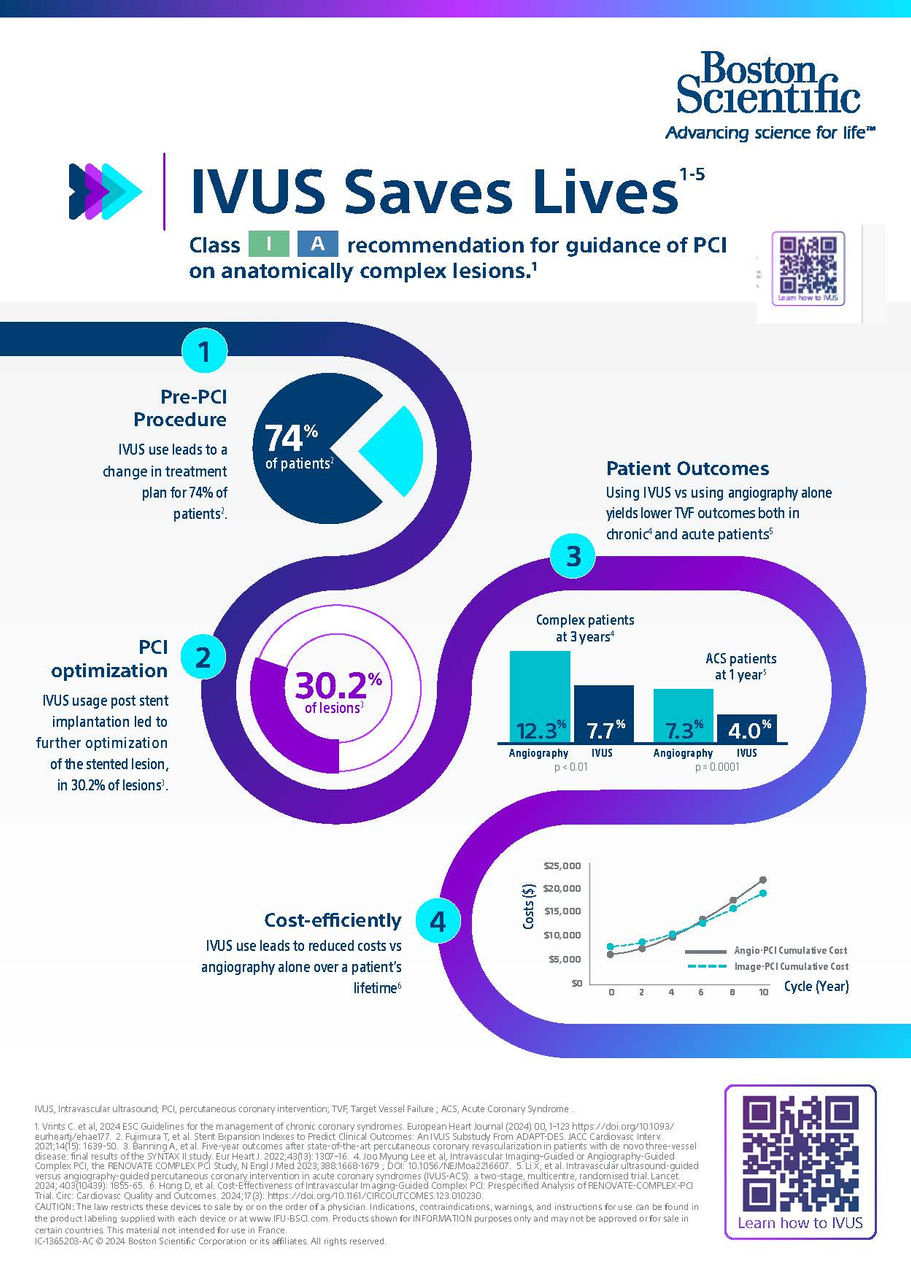
IVUS saves Lives
The 2024 ESC Guidelines rank IVUS at
class 1, level A1
The ESC has changed their recommendation for IVUS or OCT - guidance of PCI on anatomically complex lesions, particularly Left Main, true bifurcations and long lesions to class 1, level A1 . Their decision was supported by recent clinical studies such as RENOVATE-Complex PCI2 (complex lesions), IVUS-XPL3 (long lesions) and OCTOBER4 (true bifurcations) all showing positive evidence that intravasular imaging optimizes patient outcomes when compared to angiography alone.
The infographic one-pager available for download, highlights the key IVUS data available.
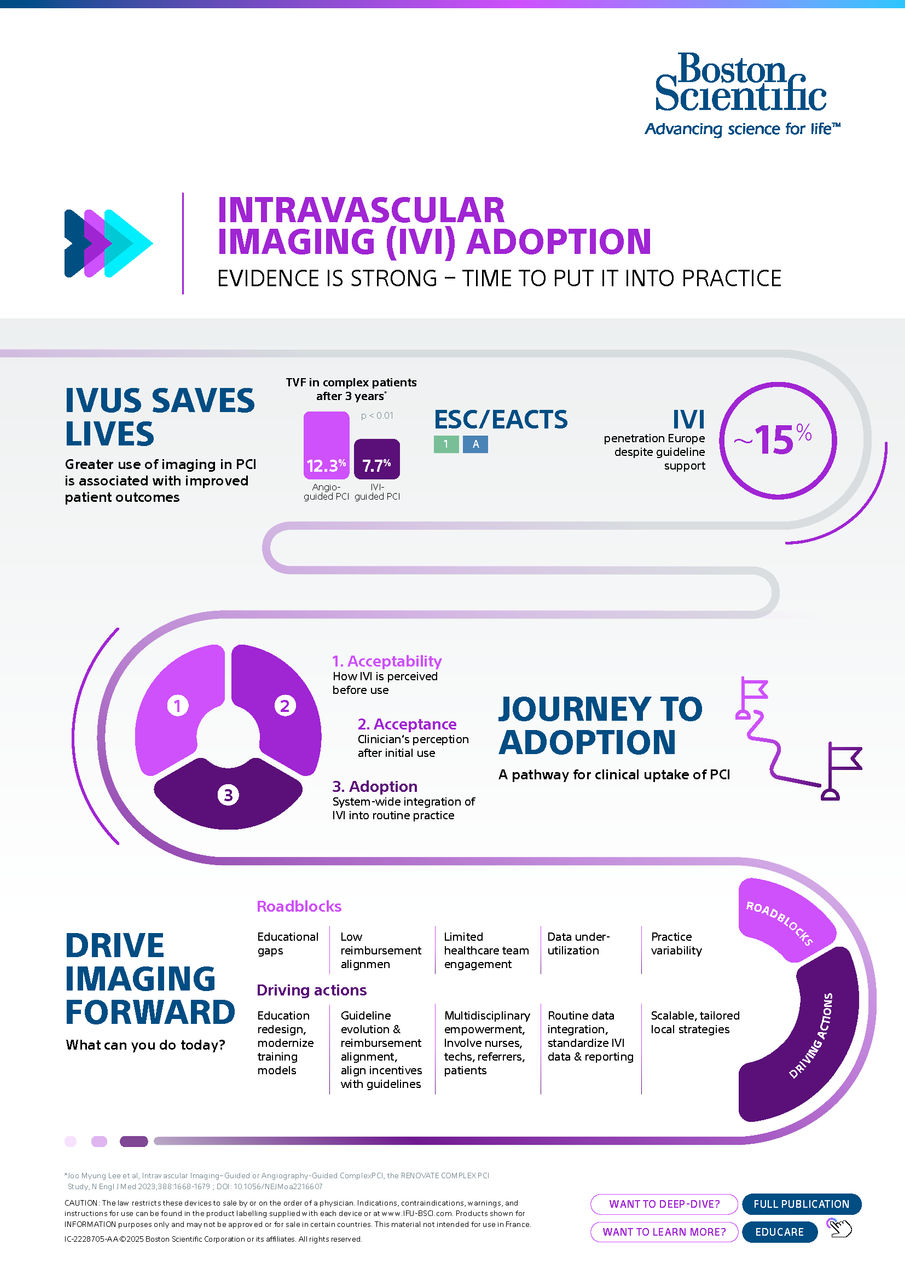
Intravascular Imaging (IVI) Adoption
The evidence is clear, using IVI in your PCI procedures will enhance patient outcomes5. But its adoption in clinical practice is still low with only 15% in Europe using IVI in the Cath Lab regularly. As an interventional cardiologist, you can choose to be part of the change movement to enhance IVI adoption. You can act in your own Cath Lab, understanding and addressing the main barriers, like educational gaps, reimbursement systems and practice variability.
Download the clinical one-pager or read the full article to explore the journey to adoption and discover practical steps you can take today to put evidence into practice.
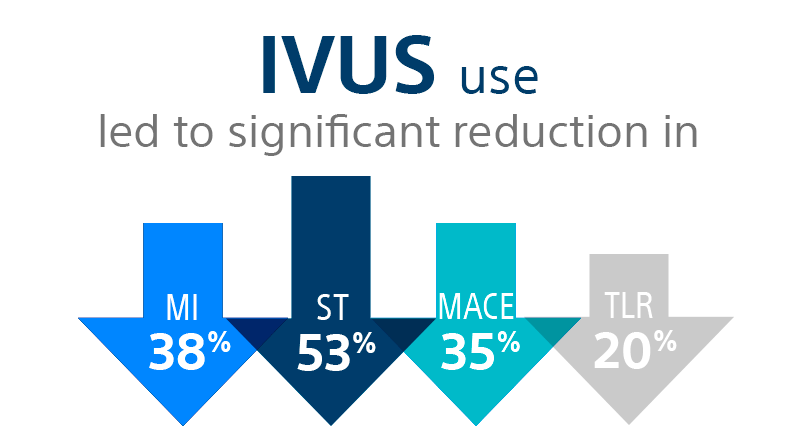
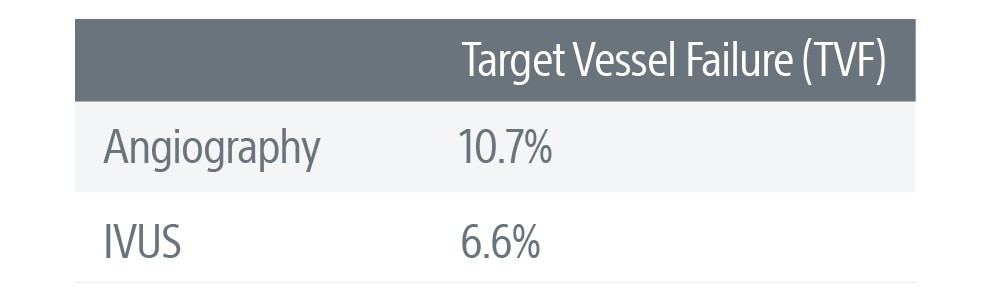
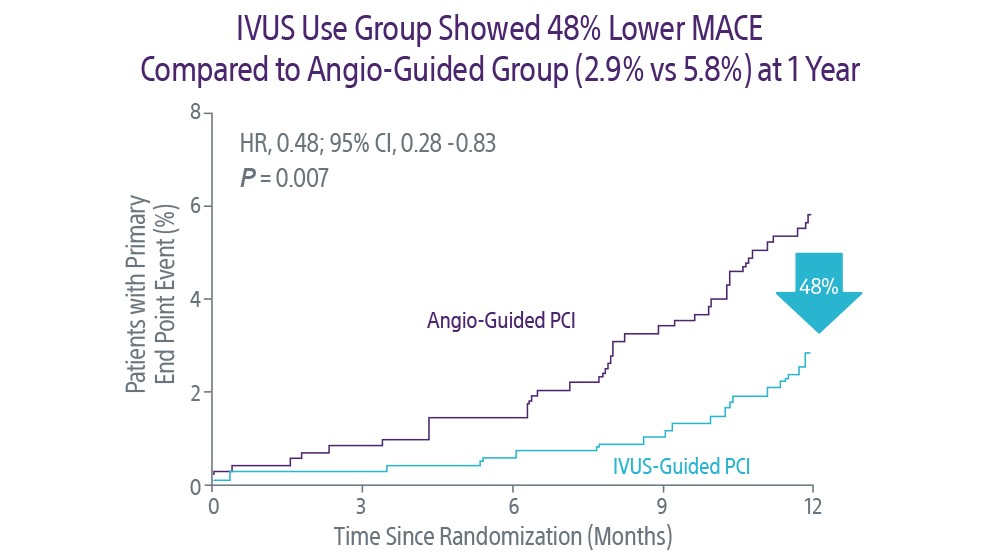
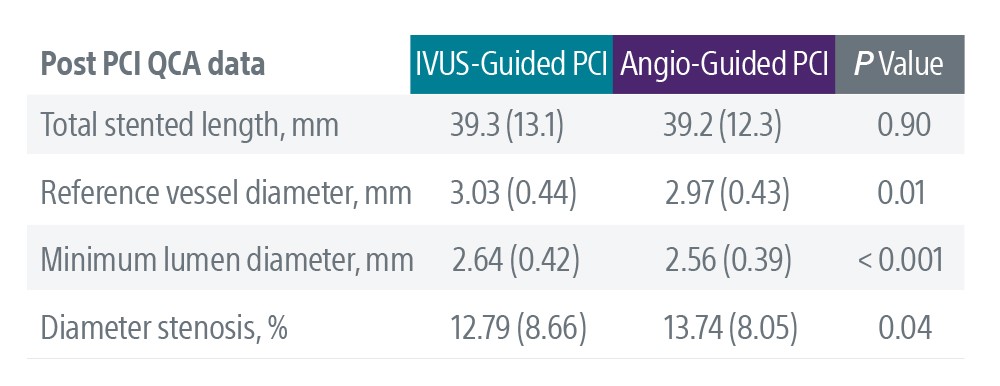
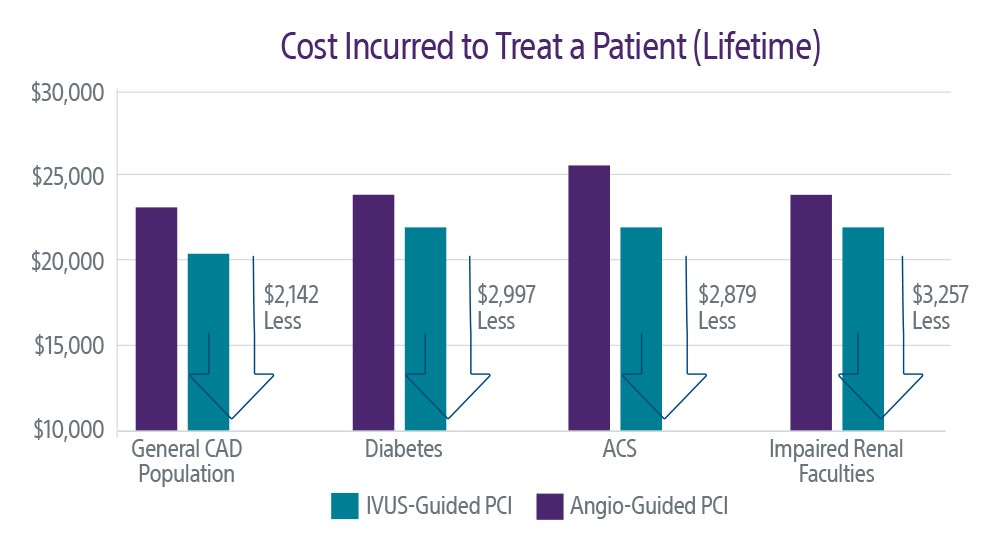
IVUS Guidance Optimizes Coronary Outcomes
Intravascular ultrasound (IVUS) is a core tenet of the SYNTAX II 6 methodology for state-of-the-art PCI. The study’s five-year outcomes, along with several other highly-regarded trials, demonstrate that IVUS visualization optimizes long-term outcomes by enabling more comprehensive procedure planning, execution, and assessment.
- Minimum lumen area in the stented segment more than 5.00mm2 or 90% of the minimal lumen area at the distal reference segments
- Plaque burden 5mm proximal or distal to the stent edge <50%
- No edge dissection involving the media with length more than 3mm
- Statistically higher MACE rates when stent deformation occurred
- Stent deformation at 3 years: 28% MACE
- No stent deformation at 3 years: 13% MACE