ClinicalEVIDENCE newsletter #3 – July 2023
Welcome to the ClinicalEVIDENCE newsletter, your go to source for the latest clinical data on heart diseases, diagnostics, and monitoring.
Our aim is to provide you with cutting-edge information that will keep you up-to-date on the most recent advancements in the field of heart failure management.
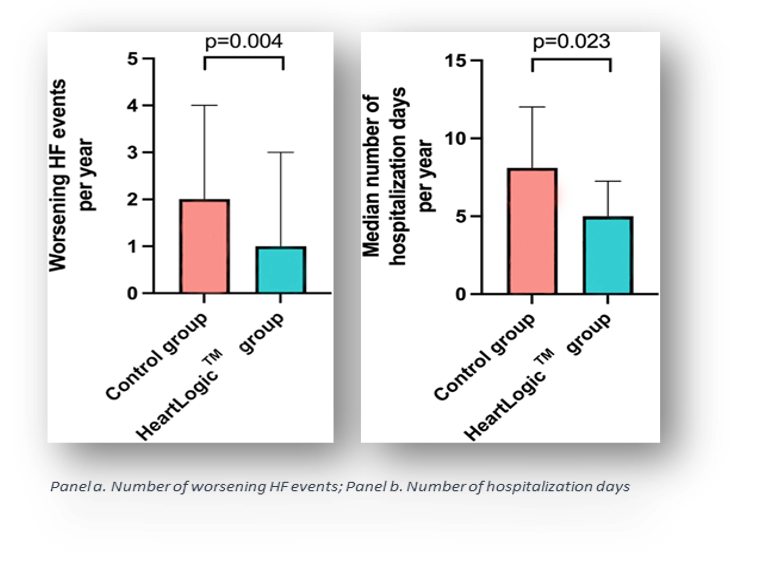
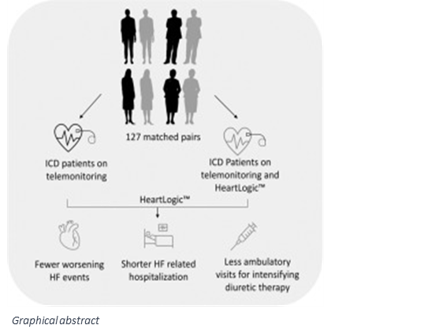
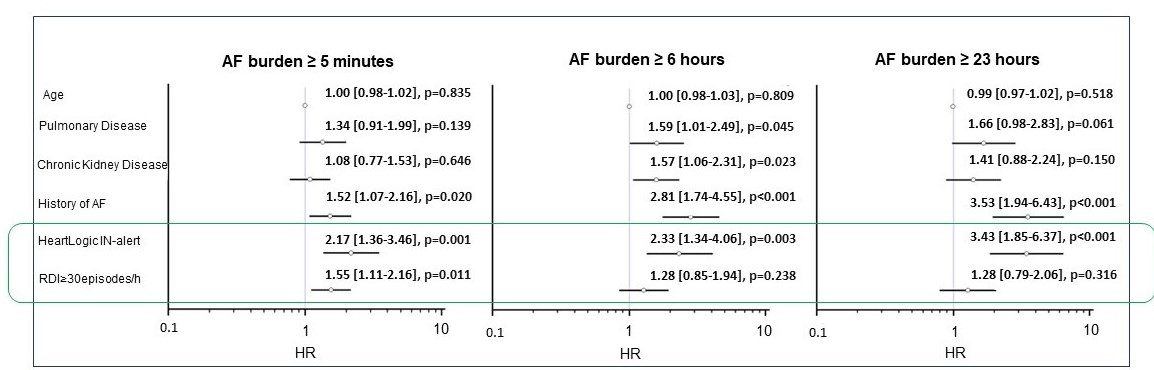
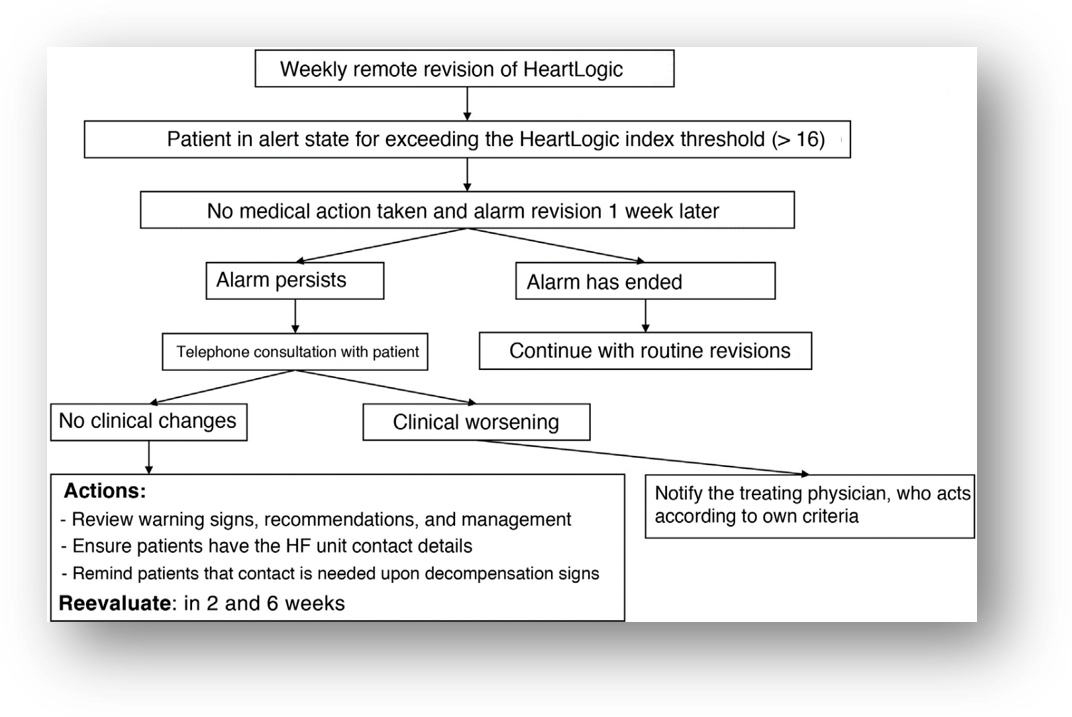
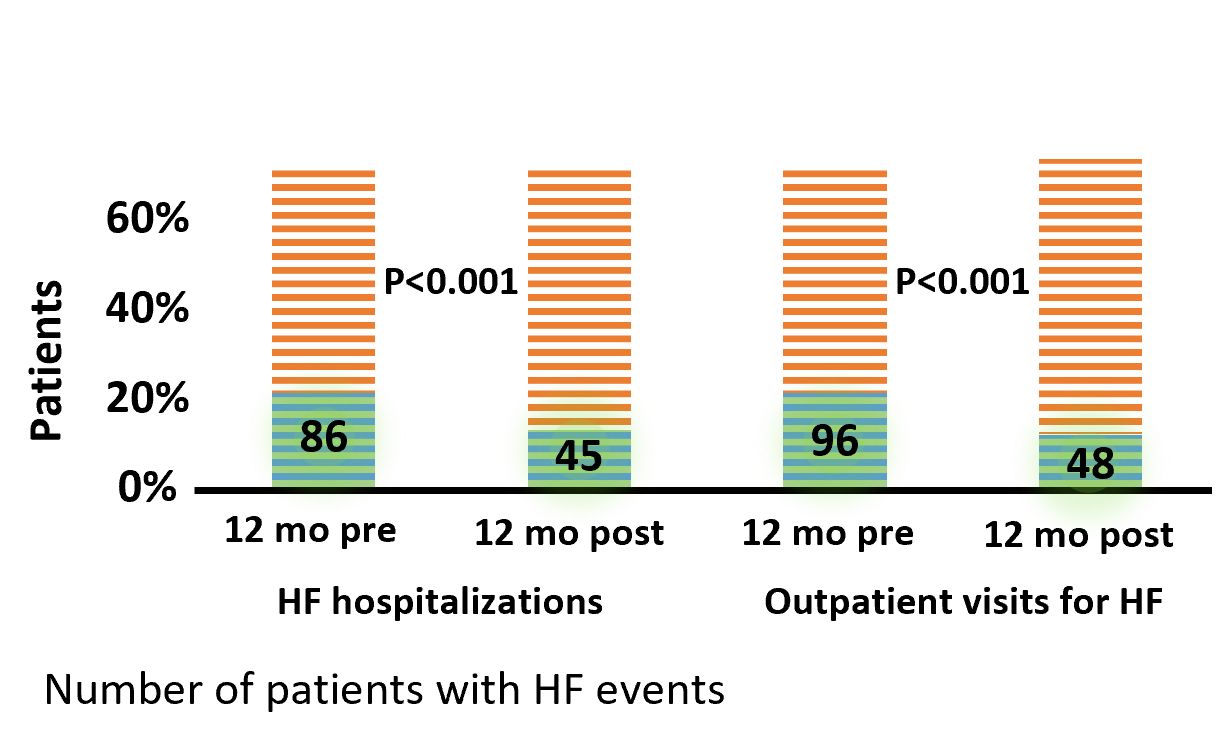
In this issue, we are excited to have the opportunity to share the key messages from the two latest publications on HeartLogicᵀᴹ.
We will also provide you with the highlights of the abstracts presented at the most important congresses earlier this year.