Rotablation and Cutting Balloon® as complementary techniques in treatment of heavily calcified lesions
Serra, A. Jimenez, M., Millan X., Gheorghe L., Bajo E., Delgado, J.
Case Highlights
- The use of Rotational Atherectomy as a primary strategy for treating calcified lesions in order to facilitate optimal stent delivery and expansion
- How to set-up the Rotablator™ system and procedural recommendations
- Complication management: “Ping-Pong” technique as one of the strategies to free an entrapped burr
- Concomitant use of rotablation and Flextome Cutting Balloon™ Device prior to stenting to enhance the vessel preparation
Patient History
- Male 72 year-old
- Risk factors: hyperlipidaemia, former smoker
- Prior cardiac history: STEMI (2011): 3 vessel disease: 2nd marginal 100%(culprit lesion), distal RCA 60%, Mid LAD 85%.
- PPCI of 2nd marginal: DES 2,5x15 mm DES.
- Staged PCI of proximal-mid LAD: Rotational atherectomy and DES 2,75x15 mm DES.
- Recent admission for chest pain (Stable angina CCS2) with optimal medical treatment.
- ETT: LVEF 50%, with inferior and anterior hypokinesia.
Clinical Presentation
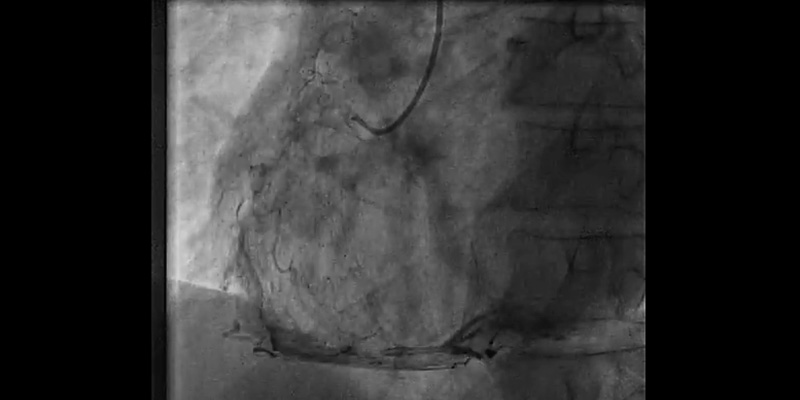
Coronary Angiography
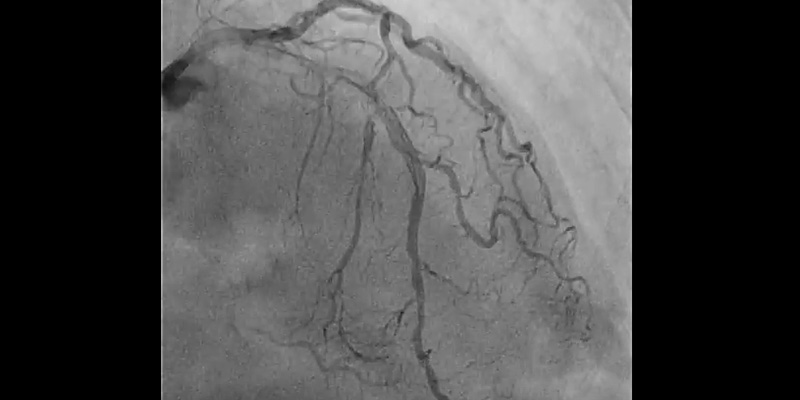
- Right coronary artery showed significant stenosis in the proximal segment (70%), severe calcification of the proximal and mid segments, and critical stenosis in the distal segment (95%)
- LAD with stent in the proximal segment without restenosis. Mid LAD showed severe calcification with a significant stenosis - 85% (Medina 1-0-1) involving the diagonal ostium
- Circumflex artery: first obtuse marginal, 70% stenosis. Second obtuse marginal with implanted stent, without restenosis
Syntax score I: 20, Syntax score II PCI: 28.2, CABG 30.5.
Decision
Percutaneous revascularization with use of Rotablator to treat the severely calcified LAD lesion
Strategy
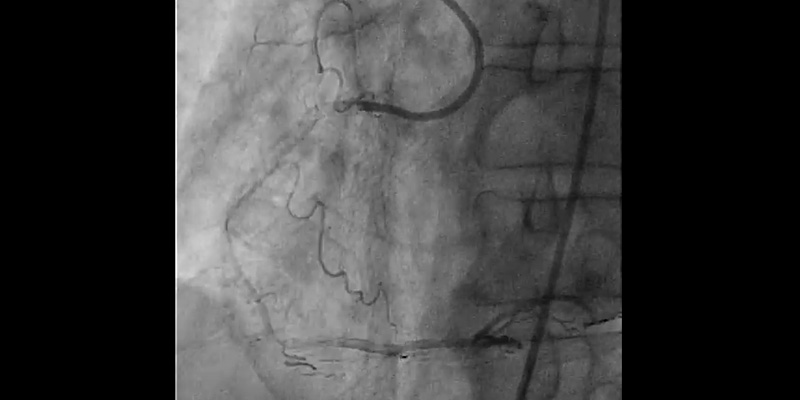
- Step 1: Routine PCI of proximal and distal RCA.
- Step 2: Vessel preparation (Rotational atherectomy + Cutting BalloonTM) of mid LAD to facilitate subsequent balloon dilatation and SynergyTM stent implantation.
Case challenges
- Severe calcification of proximal and mid segments of the LAD and tortuosity at lesion site.
- The target lesion involves diagonal branch bifurcation.
PCI with plaque modification of mid LAD
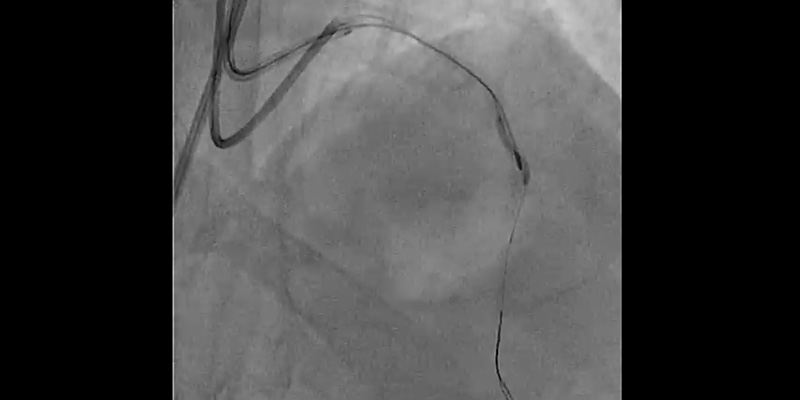
- Femoral access: 7 Fr. EBU4 7F Guiding catheter.
- The LAD was first wired with a hydrophilic wire and then exchanged for the Rotawire™ Extra Support guide wire using a microcatheter.
- Rotational atherectomy with a 1.25mm burr: A 1.25 mm burr was selected due to the severity of the stenosis and calcium. Individual rotablation runs (30-45 sec) were done with a burr speed of 165,000 rpm
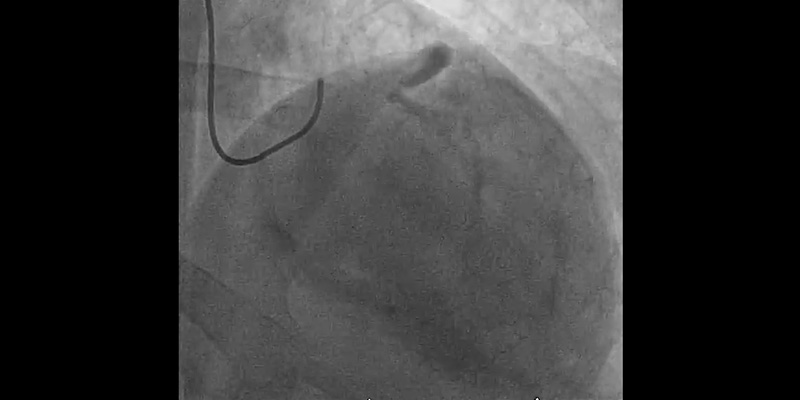
- Due to severe calcification and vessel angulation, the burr jumped distal to the lesion even with a gentle manipulation of the system. Withdrawal of the burr was unsuccessful. The system was put into Dynaglide which also resulted in an unsuccessful retrieval attempt. A hydrophilic guidewire was placed parallel to the RotablatorTM catheter but a balloon could not pass through the 7Fr femoral guiding catheter.
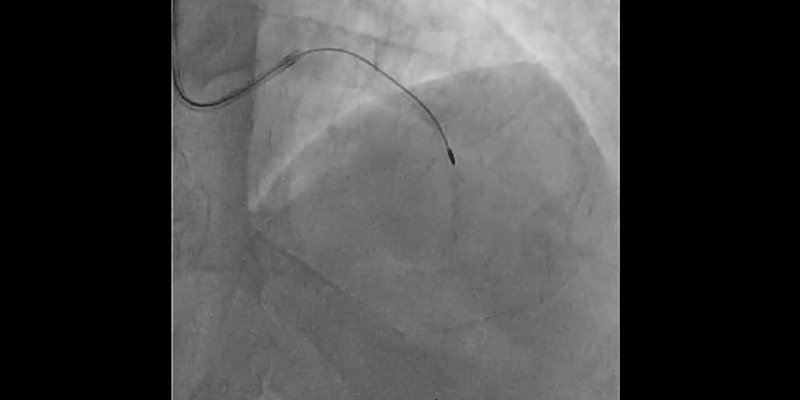
- Complication management strategy: A “Ping-Pong” technique was performed. The LM was engaged with a 6F radial EBU guiding catheter, while pulling back the 7Fr catheter a few centimetres. A hydrophilic wire was placed in the distal LAD parallel to the rotablator catheter and sequential dilatations with 1.2mm and 2.0mm balloons were performed at the site where the burr was trapped. This dislodged the burr, allowing it to be easily withdrawn.
- 2nd Rotational atherectomy with a 1.25mm burr: RotawireTM was placed again through the 6Fr radial catheter and rotablation was performed with a new 1.25 mm burr. Multiple runs were completed until there was no resistance through the lesion or drop in RPM.
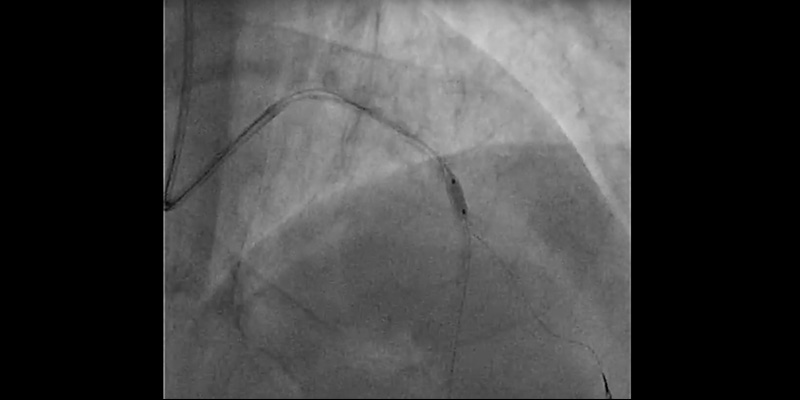
- Control angiography showed dissection at bifurcation involving the ostium of the first diagonal branch. With the help of a dual-lumen catheter, a second wire was placed into the diagonal branch.
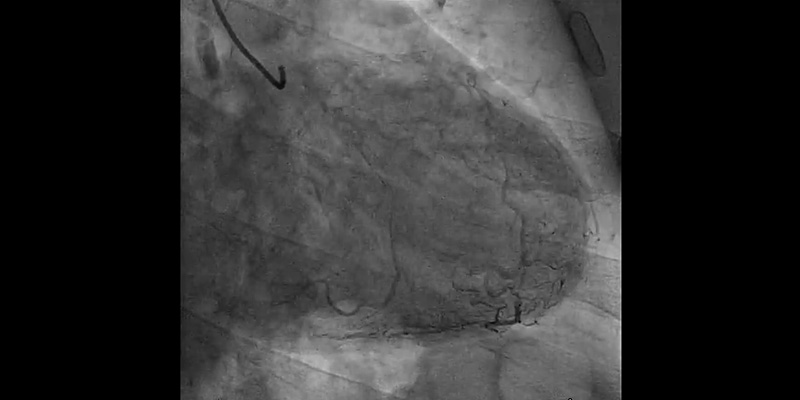
- IVUS (OptiCrossTM IVUS catheter) showed plaque rupture after rotablation at different levels. However, a calcium ring of more than 270º was observed at the site of maximum plaque.
- For this reason, plaque modification was completed with a 2.5x6mm FlextomeTM Cutting BalloonTM.
- Finally, provisional stenting of mid LAD (2.75x24 mm Synergy stent) and post-dilatation with a NC EmergeTM (3.0x12 mm) showed a good result when confirmed with IVUS. Dissection on the diagonal was still present, with a TIMI 3 flow.
KEY LEARNINGS
ROTATIONAL ATHERECTOMY
- RA is recommended for the treatment of heavily calcified lesions. Although current practice tends to use RA as a bailout only after inadequate dilation of the vessel.
- In this case severe calcification involving both sides of the arterial wall was clearly identified on angiography, therefore rotablation was used as a primary strategy for plaque modification in order to facilitate procedural success. Trying to dilate these types of lesions with a balloon catheter only can result in unsuccessful dilatation and also dissection compromising the procedural success, while increasing time and costs.
- Sufficient planning and strategy is mandatory for rotablation procedures. Nowadays, we tend to choose small burr sizes
to achieve plaque modification, 1.25 mm or 1.5 mm burrs are common sizes while the 2.0 mm burr and larger are seldom
used. Small burrs, short runs and timing between runs (according to the presence or absence of chest pain and EKG
changes during rotablation) drastically reduce the probability of the most common complication seen with rotablation:
slow flow or no reflow.
IVUS AND CUTTING BALLOON™
- IVUS is an essential tool in conjunction with rotablation. Not only to evaluate the size of the artery and plaque characteristics, but also to identify the need to complete the procedure with a non-compliant balloon or with a cutting balloon if the ring of calcium is still present.
- The Flextome™ Cutting Balloon™ Device was successfully used after rotablation prior to stenting to enhance the vessel preparation. The precise cutting action of Flextome™ Cutting Balloon™ changed the lesion compliance, enabling uniform stent expansion that will lead to a good long-term result after DES implantation
COMPLICATION MANAGEMENT
- Burr entrapment is a rare complication, which can be solved with different strategies. In this case we did the Ping- Pong technique with balloon dilatation, which is a safe way to recapture the burr. Our advice when a complication like this occurs is to keep calm and use a staged strategy to solve it.
View live case video (in Spanish)
Note: You must be a Incathlab member to watch the video without any restrictions. Registration is free.
Join Our Complex PCI Community
Education & Training
Educare offers a comprehensive suite of education and training programs for Complex PCI.
Learn MoreResources
Download Case Study