Interventional Endoscopy
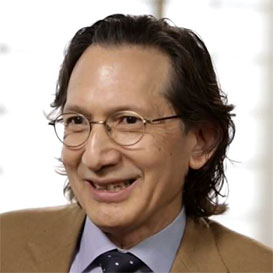 By Dr. Kenneth Binmoeller
By Dr. Kenneth BinmoellerFounder and Director of Interventional Endoscopy Services
California Pacific Medical Center in San Francisco
Interventional endoscopy is an approach. It is not specific to any organ such as the esophagus, the colon or the pancreas. It is also not specific to any imaging modality that we use to guide procedures. Interventional endoscopy is about hand-eye coordination, understanding the tools used and being able to deliver and execute the maneuvers with great precision and accuracy. With endoscopic ultrasound, we use ultrasound as another imaging modality to guide procedures.
Innovation should be part of every interventional endoscopist’s repertoire and daily practice. It starts with identifying the limitations and needs we come across during our practice. We should always ask ourselves, how can I make this method better to improve outcomes and what type of tool would enable me to do something that I cannot do currently?
These are all skill sets in terms of using the tools and imaging modalities, and they complement one another. To be a universal interventional endoscopist, you need to integrate these skill sets, and that’s when you can dramatically change the clinical course of a patient.
Pseudocyst drainage is a good example of being able to change the clinical course of a patient. Say, for example, you have a patient with pancreatic enzymes that are digesting the small intestine, leaking out into the retroperitoneum, and compressing neighboring organs. You insert a needle and place a stent, and the contents which are often infected, flow out. You’ve just changed the patient’s course of treatment.
Innovation in Practice
Innovation should be part of every interventional endoscopist’s repertoire and daily practice. It starts with identifying the limitations and needs we come across during our practice. We should always ask ourselves, how can I make this method better to improve outcomes and what type of tool would enable me to do something that I cannot do currently?
Interventional endoscopists tend to look for tools that are logical, controllable and that perform in a predictable manner. I knew that to forge the new frontier of transluminal therapy; we needed dedicated tools to perform EUS guided transluminal therapy safely and efficiently. In 2004, I founded Xlumina and developed AXIOS™, a lumen apposing stent to address this need. At the time, it was unheard of to have EUS guided transluminal therapy outside of the walls of the GI tract. Today, transluminal therapy is becoming common.
Shift to Less Invasive
Interventional endoscopy is starting to compete with surgery. A good example is pseudocyst drainage which used to be a surgical procedure, but now endoscopic drainage is becoming a more preferred method. That’s where I see the future—interventional endoscopy will become increasingly competitive and the preferred approach to disease.
20mm AXIOS™ Stent & Electrocautery Enhanced Delivery System

More Perspectives
Quality Repairs for Flexible Endoscopes: Why ISO Certification Is Important
The Training Physicians Want for Long-term Success
Biliary Stricture Management Algorithm using RFA and Stent Placement
Educare
To explore in-depth physician-led lectures, procedural techniques and device tutorials, visit Educare.
Get started














