Diagnosing and Treating a Patient with Mirizzi’s Syndrome using Cholangioscopy with EHL and SpyGlass™ Retrieval Basket
 Navin Kumar, M.D.
Navin Kumar, M.D.Digestive Disease Center
Highland, IN
Patient History
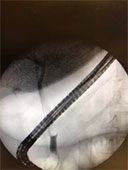
Figure 1
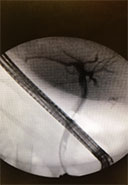
Figure 2
Procedure
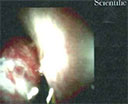
Figure 3
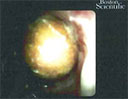
Figure 4
Figure 5

Figure 6
Outcome
More Case Studies
Direct Endoscopic Visualization via Cholangioscopy Before and After Radiofrequency Ablation
Educare
To explore in-depth physician-led lectures, procedural techniques and device tutorials, visit Educare.
Get started














