Ultrasound-assisted Thrombolysis treatment is a minimally invasive system for dissolving thrombus. Learn more how its targeted ultrasound waves accelerate thrombus dissolution.
The Acoustic Pulse difference
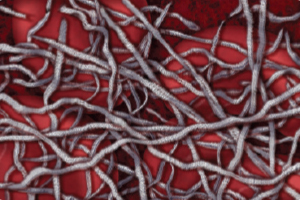
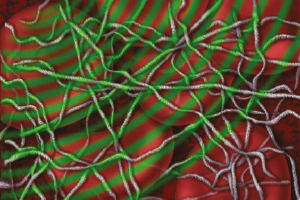
Acoustic Pulse Thrombolysis is an ultrasound-assisted treatment that is a minimally invasive system for dissolving thrombus. The ultrasonic core generates an acoustic field which greatly accelerates lytic dispersion by driving the drug deeper into the clot and unwinding the fibrin to expose plasminogen receptor sites.
Acoustic Pulse Thrombolysis Treatment
- Speeds time-to-dissolution.12
- Increases thrombus removal and clinical improvement compared to either standard catheter-directed therapy (CDT) or thrombectomy.1
- Lowers the risk of bleeding and other complications.1,3
More Effective Drug Delivery
- Reduces dosage requirements by as much as 68% compared to standard CDT.3
- Requires up to 4x less drug dosage than systemic delivery.5,6
- Reduces RV/LV ratio with as little as 8mg total tPA used in combination with EKOS therapy.1
Acoustic Pulse Thrombolysis Treatment
- 48% greater drug absorption within 1 hour.7
- 84% greater drug absorption within 2 hours.7
The EKOS System’s targeted ultrasound waves accelerate thrombus dissolution by unwinding the fibrin matrix.
Lower Patient Risk. Higher Procedure Predictability.
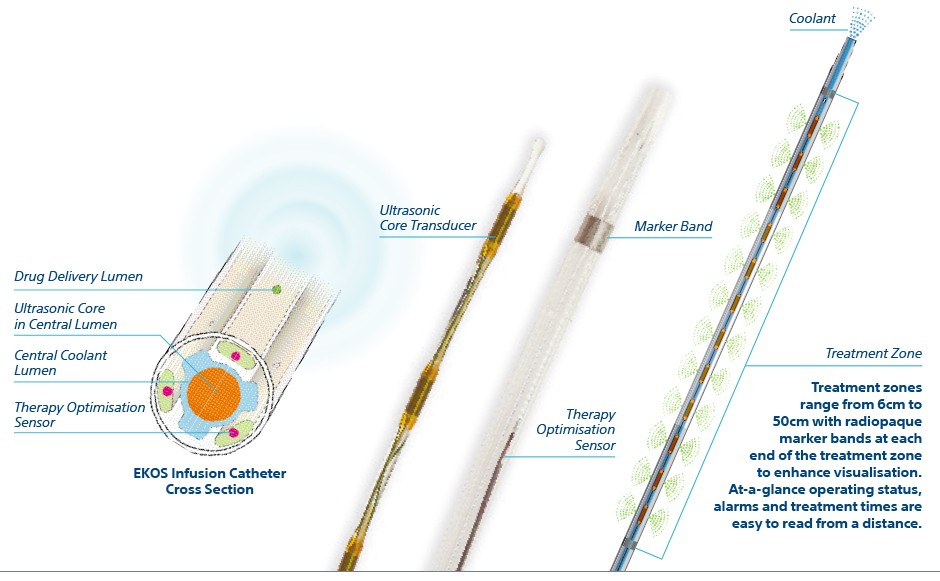
The EKOS™ Endovascular System includes an ultrasonic core within an infusion catheter and control unit.
Targeting the Thrombus, Safely
With EKOS Acoustic Pulse Thrombolysis treatment most of the drug remains in the thrombus and you can typically use less lytic. It dissolves the thrombus without damaging vessels, valves or walls.3, 9 There is no mechanical disruption resulting in distal embolisation.10 The EKOS System’s safety and efficacy is supported by Level 1 and Level 2 data.5, 6, 11, 12, 13

References:
1. Lin, P., et al., “Comparison of Percutaneous Ultrasound-Accelerated Thrombolysis versus Catheter-Directed Thrombolysis in Patients with Acute Massive Pulmonary Embolism.” Vascular, Vol. 17, Suppl. 3, 2009, S137–S147.
2. Litzendorf, M., et al., “Ultrasound-Accelerated Thrombolysis Is Superior to Catheter-Directed Thrombolysis for the Treatment of Acute Limb Ischemia.” Journal of Vascular Surgery, Jun 2011; 53(Suppl S), p106S-107S.
3. Parikh, S., et al., “Ultrasound-Accelerated Thrombolysis for the Treatment of Deep Vein Thrombosis: Initial Clinical Experience.” Journal of Vascular and Interventional Radiology, Vol. 19, Issue 4, April 2008, 521–528.
4. Lin, P., et al., “Catheter-Directed Thrombectomy and Thrombolysis for Symptomatic Lower-Extremity Deep Vein Thrombosis: Review of Current Interventional Treatment Strategies.” Perspectives in Vascular Surgery and Endovascular Therapy, 2010, 22(3): 152–163
5. Kucher, N., et al., “Randomized, Controlled Trial of Ultrasound-Assisted Catheter-Directed Thrombolysis for Acute Intermediate-Risk Pulmonary Embolism.” Circulation, Vol. 129, No. 4, 2014, 479–486.
6. Piazza, G., et al., “A Prospective, Single-Arm, Multicenter Trial of Ultrasound-Facilitated, Low-Dose Fibrinolysis for Acute Massive and Submassive Pulmonary Embolism (Seattle II).” American College of Cardiology 63rd Annual Scientific Session, Washington, D.C., March 30, 2014.
7. Francis, C.W., et al., “Ultrasound Accelerates Transport of Recombinant Tissue Plasminogen Activator into Clots.” Ultrasound in Medicine and Biology, 21.3, 1995, 419–424.
8. Soltani, A., et al., “Absence of Biological Damage from Prolonged Exposure to Intravascular Ultrasound: A Swine Model.” Ultrasonics, 46, 2007, 60–67.
9. Braaten, J.V., et al., “Ultrasound Reversibly Disaggregates Fibrin Fibers.” Journal of Thrombosis and Haemostasis, 78, 1997, 1063–8.
10. Wissgott C., et al., “Treatment of Critical Limb Ischemia Using Ultrasound-Enhanced Thrombolysis (PARES TRIAL): Final Results.” Journal of Endovascular Therapy, 14(4), 2007, 438–443.
11. Schrijver, A.M., et al., “Dutch Randomized Trial Comparing Standard Catheter-Directed Thrombolysis Versus Ultrasound-Accelerated Thrombolysis for Arterial Thromboembolic Infrainguinal Disease (DUET)” Journal of Endovascular Therapy 2015; 22(1):87-95.
12. Tapson, Victor, et al., “A Randomized Trial of the Optimum Duration of Acoustic Pulse Thrombolysis Procedure in Acute Intermediate-Risk Pulmonary Embolism: The OPTALYSE PE Trial.” JACC: Cardiovascular Interventions Jul 2018, 11 (14) 1401-1410.
Caution:
The law restricts these devices to sale by or on the order of a physician. Indications, contraindications, warnings and instructions for use can be found in the product labelling supplied with each device.
Products shown for INFORMATION purposes only and may not be approved or for sale in certain countries.
This material is not intended for use in France.