Medical Specialties > Interventional Radiology > Ablation Solutions > Cryoablation Indications > Prostate Cancer
Prostate Cancer
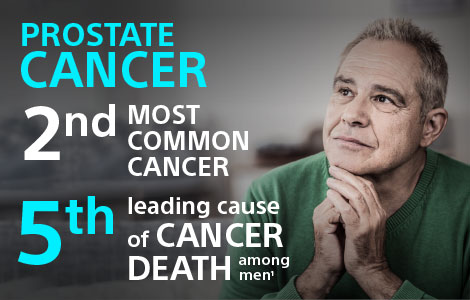
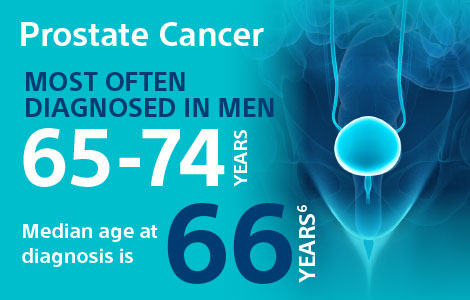
Prostate cancer is the third most common cancer worldwide (7.3% of total new cases in 2020), with an incidence rate that varies according to geography from 6.3 to 83.4 per 100,000 men. The highest rates are found in Northern (83.4 per 100.000) and Western Europe (77.6 per 100.000). It is the second most common cancer in men and the fifth leading cause of cancer death.1
Prostate cancer occurs when cells inside the prostate gland start to grow out of control, and, in the majority of cases, it is diagnosed as adenocarcinoma.2
Depending on how far the disease has progressed, prostate cancer is staged from I through IV: 3
- Stage I: cancer is on one side of the prostate;
- Stage II: cancer has spread but it remains confined to the prostate gland;
- Stage III: cancer is in both sides of the prostate (3A), or it has spread outside the prostate gland to nearby tissues (3B, 3C)
- Stage IV: cancer has reached the lymph nodes or has spread to other body parts.
Subtypes
Subtype |
Incidence |
Description |
Use of CA |
|
Adenocarcinonoma |
Acinar adenocarcinoma (AAC) | ~90% A |
Acinar adenocarcinoma (AAC) is the main subtype of prostate cancer. It develops in the cells that line the prostate gland and mostly occurs in men aged over 60.A,B |
Cryoablation has demonstrated excellent outcomes both as a local primary treatment for early-stage prostate cancer and as a strong local
Nance M.E, et al. report two successful cases of cryoablation used as salvage therapy for recurrent prostate cancer (adenocarcinoma and squamous cell carcinoma), describing it as a treatment able to provide local tumour control.H A recent case study has demonstrated MRI-guided whole-gland cryoablation to be an effective alternative option to treat prostatic adenocarcinoma for patients who had prior pelvic surgery.I |
| Ductal adenocarcinoma (DAC) | ~5% C |
Although rare, ductal adenocarcinoma (DAC) is the second most common subtype of prostatic cancer.C It develops in the cells that line the ducts (tubes) of the prostate gland and it grows and spreads more quickly than AAC.A,B It usually occurs in men aged between 63 and 72.D |
||
| Neuroendocrine carcinoma | < 5% B (very rare) |
Neuroendocrine carcinoma can start in neuroendocrine cells anywhere in the body, rarely in the prostate.B |
||
| Transitional cell (or urothelial) cancer | Transitional cell cancer usually starts in the urethra or bladder and spreads to the prostate; it can rarely start in the prostate.E |
|||
| Small-cell carcinoma | Small-cell carcinomas accounts for ~1% of prostate cancers. It grows in small round cells in the prostate and can spread very quickly.E |
|||
| Squamous cell carcinoma | Squamous cell carcinoma is a rare (<1%) and aggressive form of prostate cancer which develops in the flat cells that cover the prostate glands.B,E |
|||
| Soft tissue sarcoma | Soft-tissue prostate cancer is extremely rare (<0.1% of the cases).B It tends to develop in the soft tissue outside the prostate gland.E |
|||
Treatment options
Local treatments
Systemic treatments
In addition, the ESMO association suggests cryoablation is a strong local salvage therapy. 4
Clinical Results – Why Cryoablation?
Explore cryoablation as a primary treatment for prostate cancer
“Focal therapy [cryoablation] offers a middle ground between these extremes [radical prostatectomy and active surveillance] by precisely targeting only the cancer-bearing part of the gland while preserving the remainder of the prostate and its delicate surrounding structures.”
Lebastchi A.H et al, 2021 12
Cryoablation has been shown to be an effective primary therapy for localised prostate cancer, both if adopted as whole-gland treatment and as a focal therapy option.7,8,9,10,11
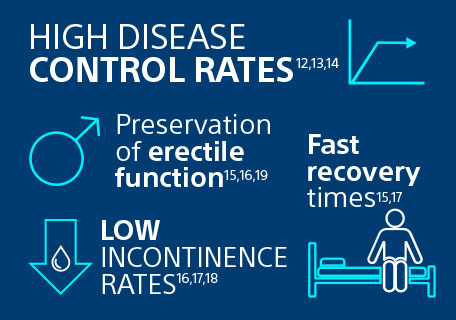
In particular, it has demonstrated excellent outcomes in terms of oncologic control 12,13,14and preservation of erectile function14,15,16; cryoablation also leads to low incontinence rates16,17,18 and a short hospital stay15,17.
Explore cryoablation as a salvage treatment for prostate cancer
“Focal salvage cryotherapy has managed to provide oncological control and maintain this patient’s quality of life in his later years”
Taimur T Shah, 2020 Charing Cross Hospital, Imperial College Healthcare NHS Trust and Imperial College London (ICL)
View Dr. Shah’s «Salvage Focal Prostate Cryotherapy» Case Study
Cryoablation is not only a successful primary therapy for prostate cancer, but it is also able to control tumours resistant to other therapies.14,20
In recent years, it has been recognised to be an effective and repeatable 22 treatment option for patients failing primary therapy, providing excellent survival outcome (74% at 5 years) and low morbidity.17,21
Our Solutions
Cryoablation is a minimally invasive treatment that uses extreme cold to freeze and destroy diseased tissue, including cancer cells. We offer a broad portfolio of Systems and Needles, that, thanks to the latest technology, provide an efficient treatment against a range of malignant and benign tumours.
Learn more about our solutions