Introducing Transoral Outlet Reduction (TORe)

Transoral Outlet Reduction (TORe) is a minimally invasive procedure designed for patients who have regained weight after gastric bypass. By tightening the connection between the stomach and small intestine, TORe helps restore portion control and supports long-term weight loss.
How the TORe procedure is performed
TORe is performed under general anesthesia by a trained gastroenterologist or surgeon, using the OverStitch™ System. The procedure involves a flexible scope inserted through the mouth, avoiding incisions and minimizing downtime. It safely restores the stomach’s restrictive function to help patients lose weight again, with most patients typically discharged the same day.
Curious to learn more about TORe? Here’s how it works:
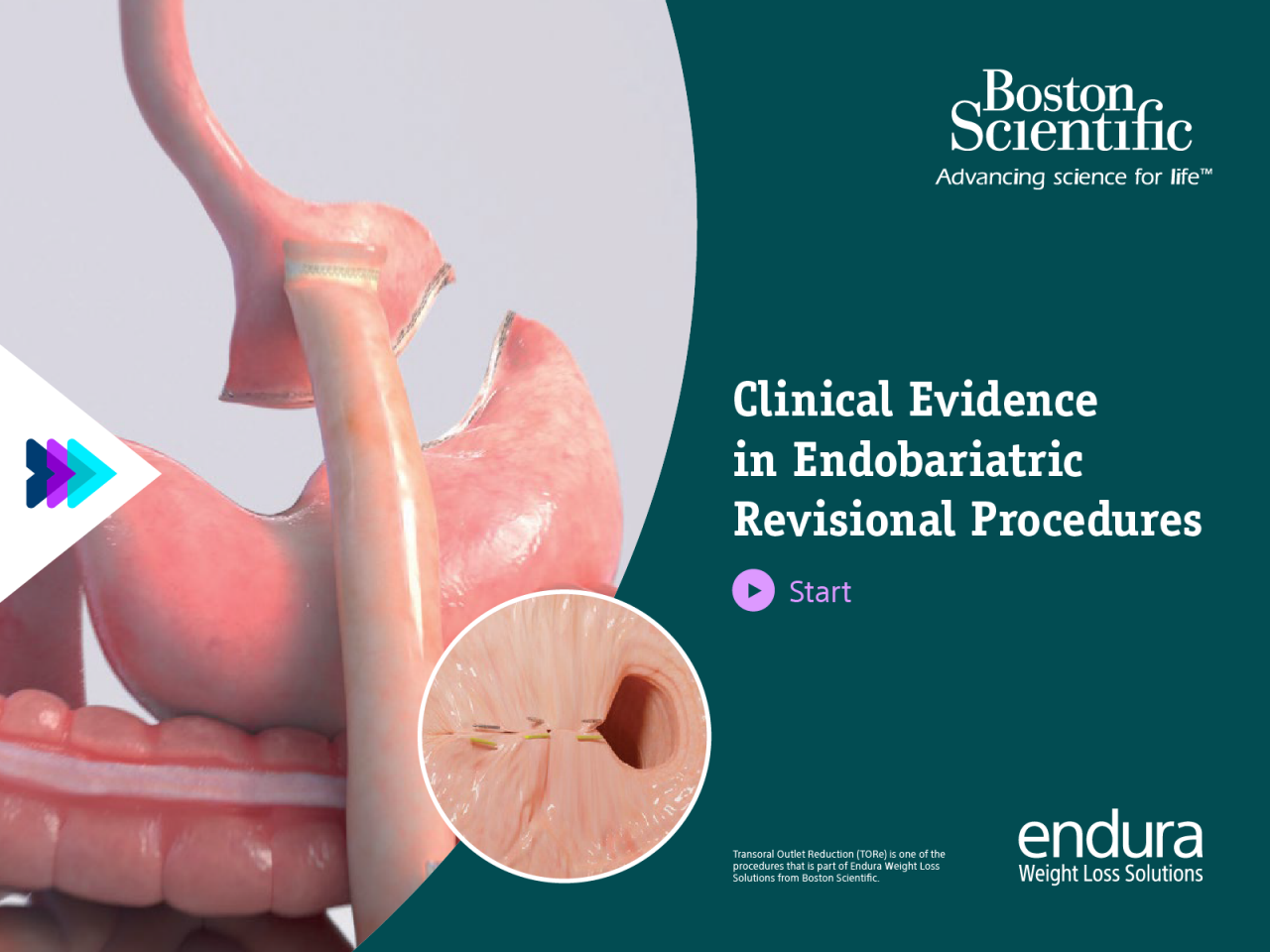
Clinical evidence
6%
Proven Weight Loss Results
In a large meta-analysis, patients who underwent TORe saw an average of 6% total body weight loss at 12 months.⁴
9-12%
Latest Technique
Latest studies using the purse-string approach report 9-12% TBWL at 12 months.5,6
5&7 y.
Support Long-Term Outcomes
Long-term studies support durable weight loss at 5 and 7 years.5,7
A comparative study demonstrated a lower rate of adverse events with TORe compared to surgical revisions, whilst achieving similar outcomes in long-term efficacy.3
| TORe n=31 | LAP n=31 | p-value | ||
| Effectiveness at 5 years | 11.5% TBWL | 13.1% TBWL | 0.67 | |
| Adverse events | 6.5% | 29.0% | 0.04 | |
| Safety profile | 0% SAE* rate | 19.4% SAE rate | 0.024 | |
Dolan, et al; Gastrointestinal Endoscopy. 2021
- Matched cohort population
- Multicentric
- Long follow-up studies: 5yrs
Key Resources
Resources for Patients
Discover comprehensive resources tailored for TORe patients across the UK, Spain, Italy, Germany, and France.
Patient Perspective: Alessia‘s TORe Journey
Listen to Alessia’s story as she shares her TORe journey.















