Atrial Fibrillation Treatments
There are a number of AFib treatments that help control your heart rate, restore a normal heart rhythm, and/or monitor your heart’s electrical activity, including:
- Drug Therapies (see hereunder)
- Internal Cardioversion Cardioversion uses electrical energy to change an arrhythmia back to a normal rhythm. By delivering a controlled electric shock through the chest to the heart, cardioverters "shock" the heart back into a normal heart rhythm.
- External Cardioversion During emergencies, the shock may be delivered through an automatic external defibrillator, or AED.
- Implantable Cardioverter Defibrillator (link to S-ICD)
- Ablation
- Catheter Ablation With cardiac ablation, a catheter is positioned inside the heart to target therapy at the tissue responsible for the arrhythmia.
- Surgical Maze Procedures
While these treatments may relieve some of your AF symptoms, they may not prevent an atrial fibrillation episode. In addition, your AFib could return without you knowing. This means there is still a risk for stroke and heart failure.
Treatments to Reduce AFIB Stroke Risk
Blood Thinners
To lower the risk of stroke, doctors may prescribe blood-thinning medications (anticoagulants) that help prevent clots from forming. These medications include warfarin (commonly called Coumadin®) and newer approved blood thinners.
Blood thinners are very effective in lowering the risk of stroke in people with AFib. Most patients can safely take these medications for years and even decades without serious side effects.
However, because anticoagulants help prevent clots by thinning the blood, they can also increase the risk of bleeding problems. Some bleeding events are minor and easily treated, like a cut taking longer to stop bleeding than normal. In other cases, bleeding can be serious and require hospitalization. Sometimes, the bleeding can be life-threatening or fatal, such as bleeding in the brain.
For some patients, the risk of major bleeding is believed to be too high for anticoagulants. When prescribing blood thinners, doctors weigh the risk of a stroke against the risk of a serious bleeding problem. These risks vary depending on existing medical conditions, family history, lifestyle, and other factors.
Implant Solution
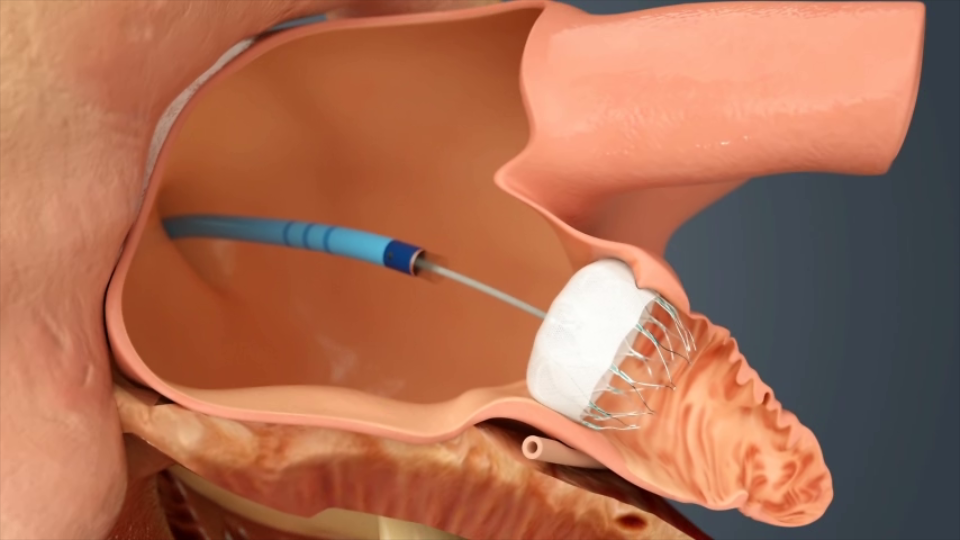
The WATCHMAN Implant offers a breakthrough approach to reducing stroke risk. Most blood clots in people with AFib develop in an area of the heart called the left atrial appendage (LAA). The WATCHMAN Implant acts as a barrier to keep these blood clots from escaping the LAA and going into the bloodstream, blocking a blood vessel, and causing a stroke.
In addition to clots traveling to the brain from the LAA, other factors can cause a stroke, including high blood pressure and narrowing of the blood vessels to the brain. The WATCHMAN implant will not prevent these other causes of stroke.

The WATCHMAN Implant doesn’t require open-heart surgery and is typically performed under general anesthesia. Like in a stent procedure, your doctor will make a small cut in your upper leg, insert a flexible tube (catheter) into a vein, and guide WATCHMAN into your heart.
Then, your doctor will cross from the right to the left side of your heart. Once WATCHMAN is in place, he or she will release the implant to permanently seal off your LAA. Over time, your heart tissue will grow over the implant.
You will need to keep taking blood thinners to help prevent a stroke until enough heart tissue grows over the WATCHMAN implant to permanently close off the LAA from the rest of your heart. Your doctor will take pictures of your heart using a TEE (transesophageal echocardiogram) to determine when the implant has properly closed off your LAA and if you can stop taking blood thinners.
Typically, patients stay in the hospital overnight and recovery takes about 24 hours. In most cases, patients can stop taking blood thinners 45 days after the procedure.