Cryoablation for Palliation of Painful Bone Metastases: The MOTION Multicentre Study
Radiology: Imaging Cancer 2021; 3(2):e200101 Jack W. Jennings, MD, PhD • J. David Prologo, MD • Julien Garnon, MD • Afshin Gangi, MD, PhD • Xavier Buy, MD • Jean Palussière, MD • A. Nicholas Kurup, MD • Matthew Callstrom, MD, PhD • Scott Genshaft, MD • Fereidoun Abtin, MD • Ambrose J. Huang, MD • Jason Iannuccilli, MD • Frank Pilleul, MD, PhD • Charles Mastier, MD • Peter J. Littrup, MD • Thierry de Baère, MD • Frédéric Deschamps, MD.
Bone is the most common site of metastatic cancer. Bone metastasis are associated with bone pain resulting in significant decreased physical function and quality of life (QOL). External beam radiation therapy is the standard for treatment of patients with painful bone metastases, along with opioids and non-opioid analgesics. Unfortunately, the time to pain relief for radiation therapy is 1-2 months and for many patients the pain can persist after radiation therapy. Cryoablation for painful bone metastases allows for rapid and durable pain palliation.
Study Objective
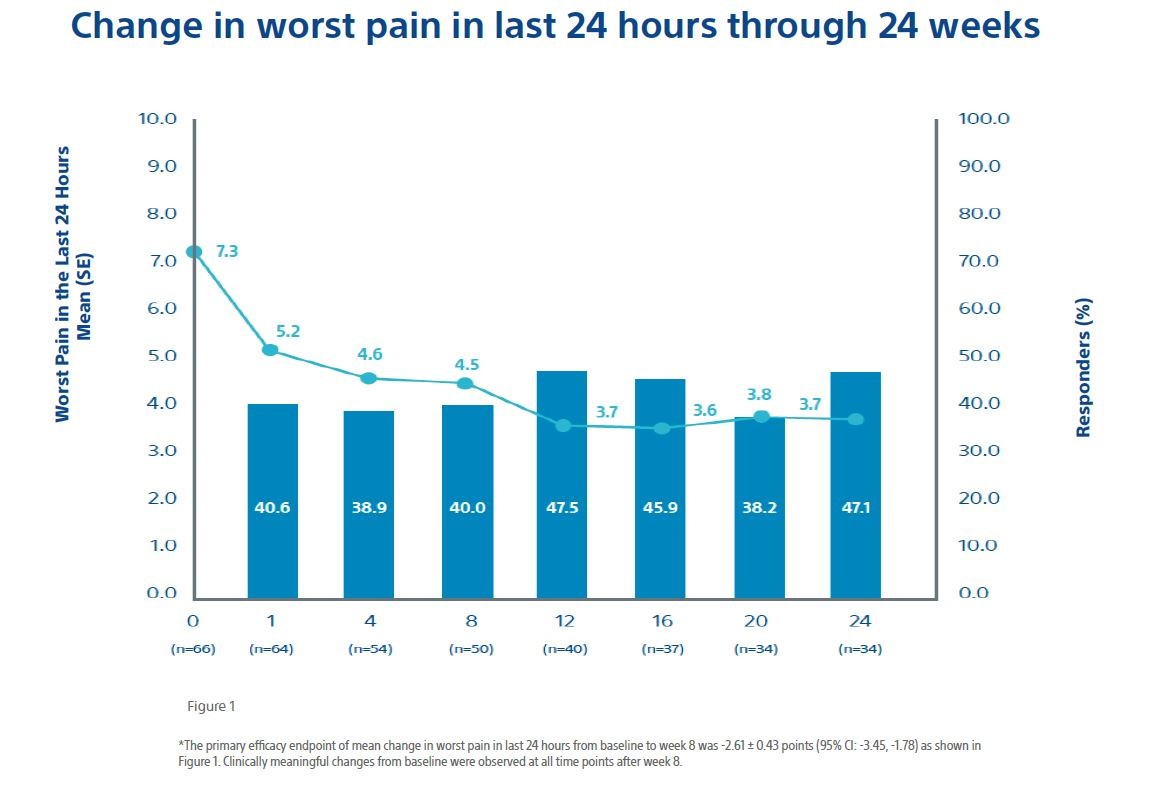
To assess the effectiveness and safety of cryoablation for palliation of painful bone metastases in participants who were not candidates for traditional pain therapies or for whom traditional pain therapies had failed to provide adequate relief. The primary objective was to evaluate the efficacy of cryoablation for pain palliation of bone metastases from baseline to 8 weeks after cryoablation in worst pain in the last 24 hours as measured by the BPI-SF scale.
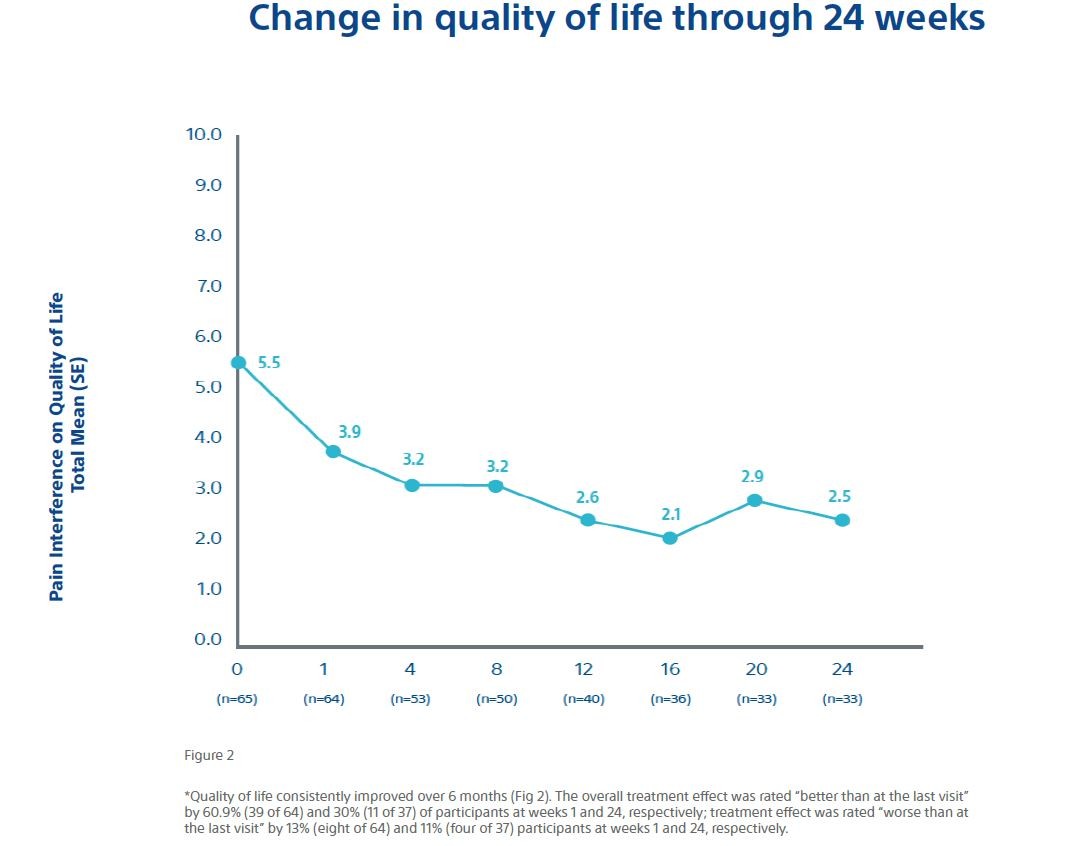
Separate evaluations of ancillary efficacy endpoints were also made through 24 weeks, including: (a) changes in worst pain scores and average pain scores from baseline; (b) change in analgesic use (both morphine equivalent daily dose (MEDD) and nonsteroidal anti-inflammatory drugs); (c) use of additional therapies for persistent or recurrent pain associated with the index tumor or new metastases; (d) quality of life (as indicated by change from baseline in overall average BPI-SF); and (e) change in Karnofsky performance status as a measure of functional impairment. The safety endpoint was the incidence and severity of procedure or device-related adverse events.
Study Design
- Multicentre, prospective, single arm, phase II study
- 11 centres: 4 in EU and 7 in US;
- Conducted from February 2016 to March 2018;
- N= 66 patients with painful bone metastases treated, 65 available for follow-up;
- Patient follow-up at 1, 4, 8, 12, 16, 20, and 24 weeks after the cryoablation procedure;
- Treatment of 1 painful bone metastatic lesion for each patient;
- Primary efficacy objective: change from baseline to 8 weeks after cryoablation in worst pain in the last 24 hours as measuredby the BPI-SF scale;
- Complications were monitored for 30 days post procedure;
- Hospital stay: median of 26.6 hours (range 19.4 – 45.8 hours).
Patient and Tumor Characteristics

Method
Study sites used a standard cryoablation protocol including two free-ze-thaw cycles.
If the operator felt that another cycle would improve coverage and local control, it was performed in select cases.
Participants were not denied needed therapy for pain; however, those who received additional targeted therapies to the index tumour were excluded. Pain improvement was evaluated using a single item from the BPI-SF questionnaire completed by participants which asked participants to evaluate the level of the “worst pain in the last 24 hours.”
The primary effectiveness endpoint was the change from pretreatment baseline rating of worst pain in the last 24 hours to post treatment week 8 rating. A clinically meaningful change for this item was defined as a reduction of at least 2 points.
Results
Sixty-six patients were included in the intention-to-treat (ITT) population in which cryoablation was attempted.
Baseline patient and tumour characteristics are shown in Table 1 with a mean patient age of 60.8 years and predominant primary cancers of lung (28/8%), breast (13.6%), and kidney (12.1%) cancer of targeted bone metastases.
The majority of patients had received previous systemic therapies (75.8%) with 42.4% of patients previously receiving radiation therapy, and only 10.6% of patients with no prior cancer treatments.
Conclusion
- The Mean pain scores improved by 2 points at 1 weeks and reached meaningful clinically relevant levels after 8 weeks and scores continued to improve throughout follow-up;
- 92% (59/64) of patients achieved pain palliation;
- Opioid doses were stabilized, and functional status was maintained over 6 months;
- Quality of life improved over the course of the study period.
Overall, the data shows a rapid and durable pain relief along with a decrease in MEDD and a corresponding increase in the quality of life for patients with bone metastases.
Cryoablation offered an alternative to opioids for pain control.
Most participants achieved their maximum palliation by
| week 1 33.9% 20 of 59 |
week 4 25.4% 15 of 59 |
week 12 15.3% 9 of 59 |