Dear HeartLogic™ users,
New articles have been published in the last weeks on the performance of HeartLogic™ in clinical practice.
Moreover, during the ESC-HF 2022 Congress that took place from 21st to 24th May in Madrid, novel data have been presented.
HeartLogicTM and Real World Care Path
Recently Dr. Feijen at al. (Leiden University Medical Center – Leiden – The Netherlands) have published on Frontiers in Cardiovascular Medicine the paper.
Performance of a HeartLogicTM Based Care Path in the Management of a Real-World Chronic Heart Failure Population
The preliminary results from this single centre experience had already been presented last year at ESC-HF Congress 2021.
The aims of this analysis were:
- to evaluate the performance of the HeartLogic-guided heart failure care path in a real-world heart failure population.
- to investigate whether the height of the index and the duration of the alert state are indicative of the degree of fluid retention.
Based on these 130 alerts, logistic regression with generalized linear mixed models
estimated that the HeartLogicTM algorithm-based care path had:
-79% Sensitivity to detect early signs of
fluid retention
-89% Specificity
-71% Positive predictive value
-91% Negative predictive value
Results:
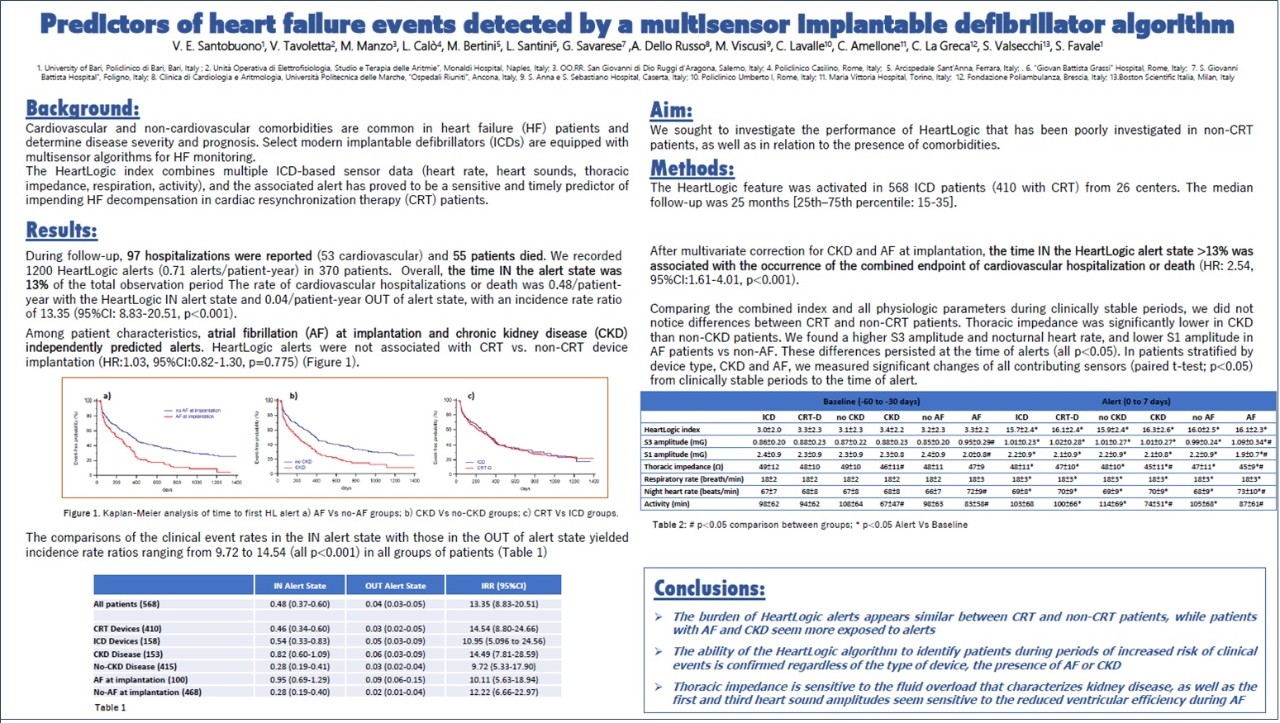
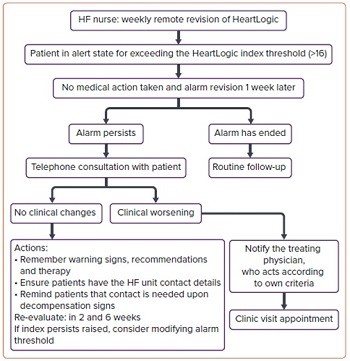
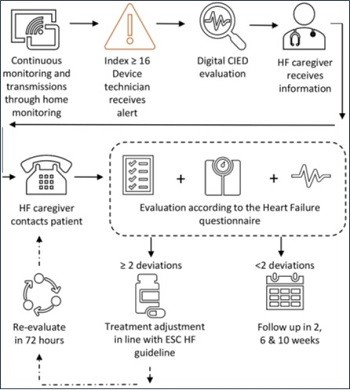
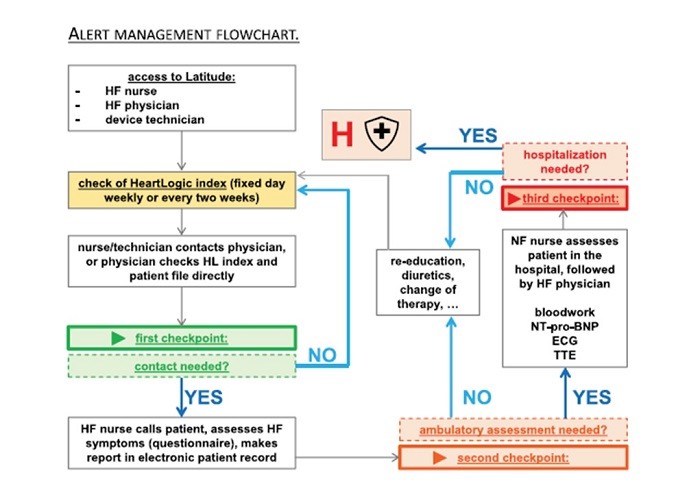
This study collected data of 107 consecutive heart failure patients with a CIED and an active HeartLogicTM algorithm. All patients underwent systematic clinical follow-up according the management flow-chart reported in Figure 1, previously described by Treskes et al. (1).
During a median follow-up of 14 months [IQR 8–23], 136 HeartLogicTM alerts occurred (0.88 alert/pt-year) with a median duration of 35 days. 92 alerts were judged TRUE POSITIVE (Figure 2).

The most common actions triggered by HeartLogicTM alerts, based on care path described, are:
-reinforcement of lifestyle advises and/or optimization of the oral heart failure medication (67%);
-administration of intravenous diuretics (24%);
-hospitalization (at least 1 night in hospital stay) for decompensated heart failure (9%).
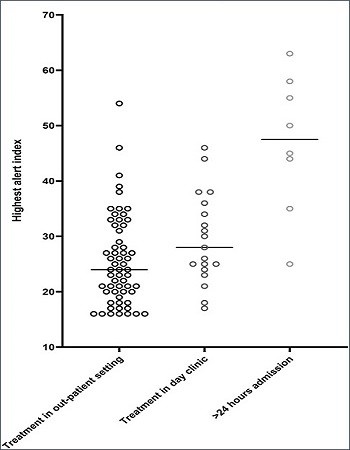
The maximal height of the HeartLogicTM index during an alert episode was lower in patients treated in the outpatient setting, than in patients intravenously treated in a day visit or in patients in whom hospitalization was required (Figure 3).
Conclusions:
Clinical Utility of HeartLogicTM
A review on multiparametric telemonitoring in heart failure and its clinical utility and use in clinical practice has been published by Dr. J. C. López-Azor et al. on Cardiac Failure Review Journal.
Clinical Utility of HeartLogicTM, a Multiparametric Telemonitoring System, in Heart Failure
The HeartLogicTM Algorithm
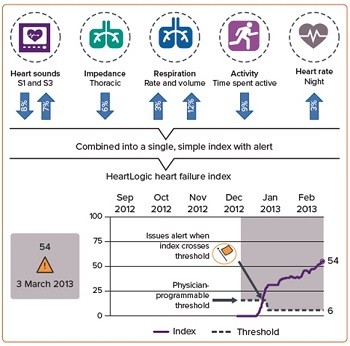
HeartLogicTM is a multiparametric algorithm implemented in certain ICDs (with or without CRT) from Boston Scientific.
HeartLogicTM allows stratification of the risk of decompensation in HF patients: is an automatic, remotely monitored system that combines trend analysis from different sensors (nocturnal heart rate, first and third heart sounds, intrathoracic impedance, respiratory rate, tidal volume and physical activity), integrating them to generate a single numerical indicator, the HeartLogicTM index.
HeartLogicTM measurements of each parameter are automatically updated daily, as is the HeartLogicTM index.
When the HeartLogicTM index exceeds a programmed threshold, an HeartLogicTM alert occurs, indicating a higher risk of decompensation (Figure 4).
Review of Clinical Evidence:
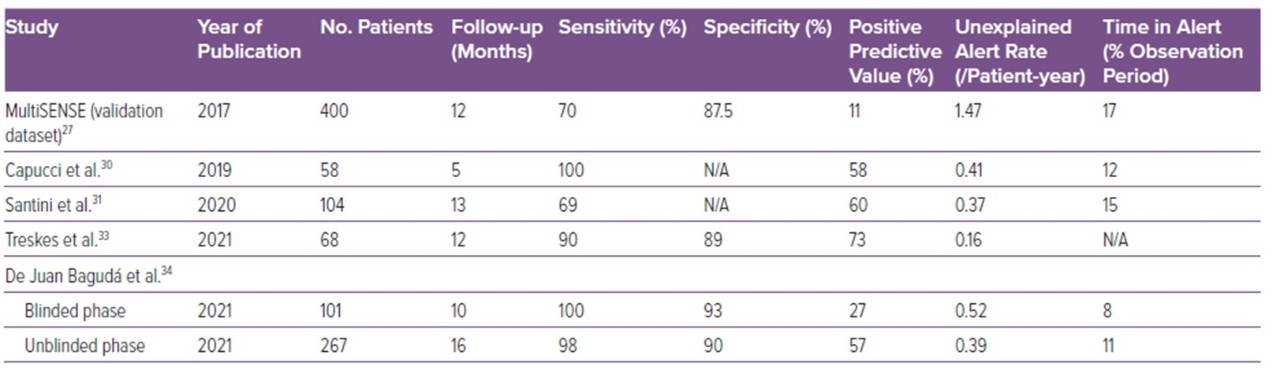
Authors, after a brief review of the MutiSENSE study, summarized the most important studies that reported the performance of HeartLogicTM in terms of sensitivity, specificity, PPV, NPV, in clinical practice.
After an HeartLogicTM alerts persisting more than 1 week, the protocol suggests a phone or face-to-face contact:
Conclusions:
It can help to reassure patients out of alert, who can be followed in a more lenient way.
HeartLogicTM review
Heggermont and Van Bockstal published in Expert Review of Medical Devices Journal a review of HeartLogicTM technical details and of main articles on the algorithm performance.
Heartlogic™: ready for prime time?
After the explanation of what HeartLogicTM is and how it works, the authors described sponsored clinical trials, published or ongoing.
The MultiSENSE trial, that developed and validated the algorithm, has been already described in multiple publications, while other two crucial clinical trials are carried out to investigate HeartLogicTM performance: the MANAGE-HF Study and Pe REEMPT-HF Study.
MANAGE-HF Study (NCT03237858): is a multicentric study investigating the potential of HeartLogicTM to prevent heart failure decompensation. Phase I results (HeartLogicTM Newsletter #3_2022) confirmed a safe integration of HeartLogicTM in clinical practice, with a significant improvement in patients' outcome.
PREEMPT-HF Study (NCT03579641): is a multicentric non-randomized study to collect device and clinical event data to evaluate extended applications of the HeartLogicTM in a broad spectrum of heart failure patients with an ICD o CRT-D device and to investigate the ability of HeartLogicTM to detect non-HF–related events in daily clinical practice.
An exhaustive table of the primary outcome and main messages of the major publications on HeartLogicTM has been included, from the MultiSENSE study published in 2017 to the 4 papers published in 2021.
Among the advantages of HeartLogicTM use, the authors mentioned the fact that the HeartLogicTM activation doesn’t require any action by the patient and the low unexplained alert burden. Moreover, they commented that it is possible to manage large groups of heart failure patients remotely, reliably and safely and that HeartLogicTM can risk stratify patients, for more efficient and effective allocation of human resources to those patients at high HF risk.
Authors also reminded that HeartLogicTM should be implemented in a multidisciplinary heart failure team and that it would be desirable to have a clear follow-up protocol in order to have alerts ‘handled’ in a structured way. An example proposed was reported in the central figure of the paper (Figure 6).
It is also strongly recommended that individual components contributing to the alert are studied in order to provide to the patient the best customized therapy for each single event.
In conclusion, it seems clear to the authors that HeartLogicTM is of added benefit to a subset of HF patients and that, when a patient is in alert state, it is important to explore not only potential causes of decompensation, but also look for non-HF-related major problems (thyroid disorders, pneumonia) that could eventually trigger decompensation.
The increasing demand for care of HF patients, and the fast evolution of telemedicine due to COVID-19 pandemic are a perfect match to promote the development, validation, and clinical application of HeartLogicTM and of telemedicine in cardiology.
ESC-HF Congress 2021
The annual congress of the Heart Failure Association of ESC took place on 21 – 24 May in Madrid.
At Heart Failure congress, scientific presentations from leading global experts covered the entire spectrum of heart failure during symposia, Guidelines in Practice sessions, how to- and case-based sessions, as well as debates.
Oral Presentations Session
Dr. Feijen from Leiden University Medical Center presented:
Correlation between height of HeartLogicTM index and severity of fluid retention: real world experience.
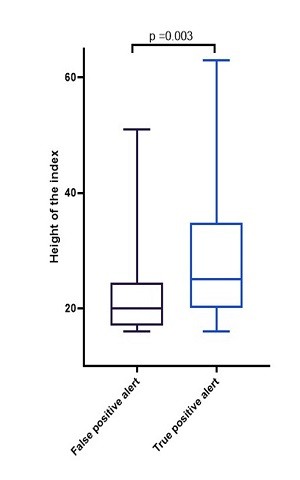
The aim of this analysis was to investigate the association between the height of the HeartLogicTM index and the severity of the fluid retention.
Consecutive heart failure patients with a CIED with an activated HeartLogicTM algorithm were included in the analysis.
All alert episodes were evaluated for signs and symptoms of fluid retention according to a defined clinical protocol: an alert was classified true positive (2 or more signs and/or symptoms of fluid retention) or false positive (1 or less signs and/or symptoms).
Median maximal alert index was 20 [IQR 17-25] in false positive alerts compared to 25 [IQR 20-35] in true positive alerts, p=0.003 (Figure 7).
Among the heart failure related alerts:
- Those treated with increased dose of oral diuretics --> maximal index median 24 [IQR 18-33]
- Those treated with a single dose of IV diuretics --> maximal index median 26 [IQR 23-38]
- Those requiring hospitalization --> maximal index median 48 [IQR 37-57], p<0.001.
The height of the HeartLogic™ index was significantly higher in patients with a true positive alert.
Patients with more severe decompensation requiring hospitalization had a significantly higher maximal HeartLogicTM index height compared to those treated in the ambulant and home setting.
For more details about this analysis, please refer to the full-length paper “Performance of a HeartLogicTM Based Care Path in the Management of a Real-World Chronic Heart Failure Population” (Feijen et al., Front Cardiovasc Med. 2022 May 6;9:883873) described before in this Newsletter.
e-Posters Session