Dear HeartLogic™ users,
We are excited to make you aware of two new and valuable HeartLogic publications and new HeartLogic content presented during last EHRA and HRS congresses!
In this issue we will deepen the content of the articles, from MANAGE-HF study and from the Italian HeartLogic Registry, both focused on the treatment administered after HeartLogic alerts. In the second part of the newsletter, we will update you about the recent interesting findings presented at EHRA and HRS Congresses.
MANAGE-HF Study: Phase I
The first publications from the Phase I of the MANAGE-HF Study has been published by Dr. Hernandez et al. on Journal of Cardiac Failure
Multiple Cardiac sensors for Management of Heart Failure (MANAGE-HF) – Phase I Evaluation of the Integration and Safety of the HeartLogic Multisensor Algorithm in Patients With Heart Failure
Methods and Objectives:
The MANAGE-HF – Phase I was a multicenter, observational study that enrolled 200 patients with reduced Ejection Fraction (HFrEF < 35%) and implanted with HeartLogic™ enabled devices. The study was designed to evaluate HeartLogic integration, utilization safety and efficacy in HF care.
Participants were monitored per routine clinical care and every 6 months per protocol to assess clinical status, events and medication changes. All patients were followed until the last participant completed the 12-month follow-up visit.
The objective was to develop an alert management guide, treatment process and evaluate associated outcomes including safety.
Results:
From August 20917 to May 2019, 200 HeartLogic patients were enrolled in 29 worldwide sites, with 191 patients completing the follow-up period.
During an average follow-up period of 20.9 months, 585 HeartLogic alert occurred (1.76 alert /pt-year) and time in alert state was 17% of total observation period.
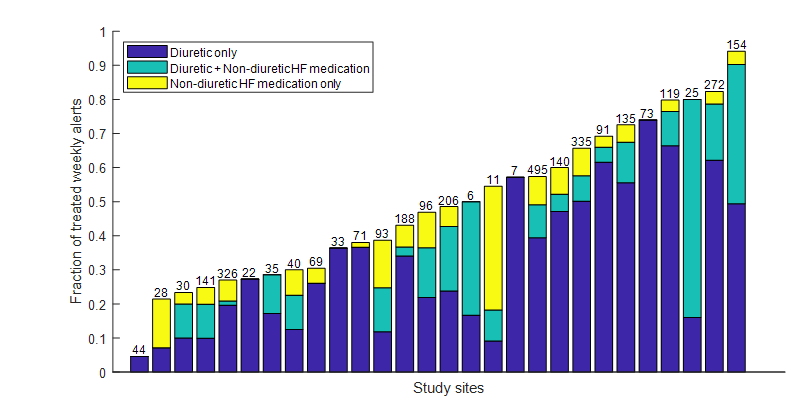
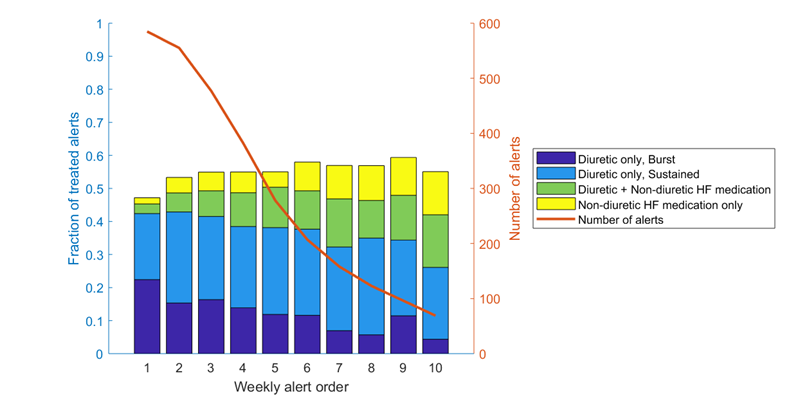
- A large variability in alert response treatment (diuretics augmentation only, diuretic + non-diuretic HF medication, non diuretic HF medication only) across sites has been observed, as reported in Figure 1A.
- The choice of response treatment, also varied by the duration of the alert case, as observed in Figure 1B.
- HF treatment was augmented during 74% of the 585 alert cases and during 54% of the weekly alerts: the majority of these changes pertained diuretics (89%).
- TFive SAEs (0.015 per pt-year) occurred in relation to alert-prompted medication changes.
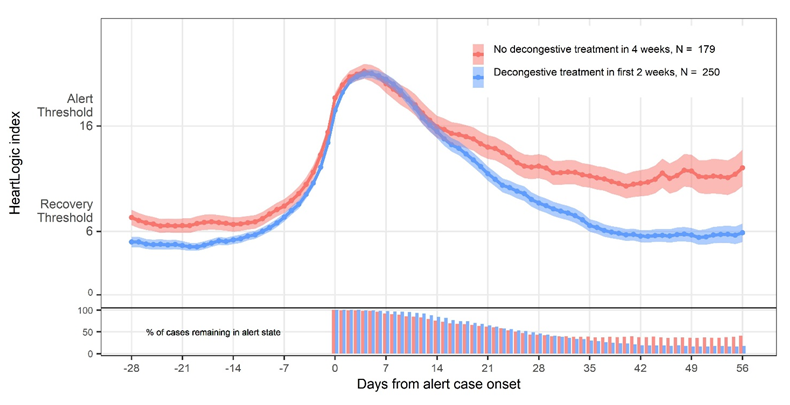
- HeartLogic Index decreased quicker and alert cases resolved quicker when decongestive therapies were given, as shown in Figure 2.
- The hospitalization rate for HF was 0.26/patient-year; HeartLogic was in alert status within 30 days preceding 83% of HF hospitalizations and 77% of intravenous outpatient treatments.
- The NTproBNP levels decreased from a median of 1316 pg/mL at baseline to 743 pg/mL at 12 months (p<0.001).
Conclusions:
- The HeartLogic multisensor index and alert algorithm management was safely integrated into clinical practice.
- The implementation of HeartLogic algorithm was associated with HF treatment augmentation, early in response to alerts, resulting in more rapid reduction of HeartLogic index values.
Decongestive treatment in HeartLogic patients
Another interesting analysis from the Italian HeartLogic Registry has been recently published by Prof. Guerra et al. on Clinical Cardiology Journal
Decongestive treatment adjustments in heart failure patients remotely monitored with a multiparametric implantable defibrillators algorithm
Most of the symptoms associated with acute Heart Failure (HF) are result of excessive fluid retention and decongestive treatment adjustments were reported, in previous experiences, to be the most frequently triggered actions in response to HeartLogic alerts.
Methods and Objectives:
Patients enrolled in this analysis were followed per clinical practice: clinicians periodically checked the remote transmissions and reviewed the patient data. At the time of HeartLogic alerts, phone assessments were performed and, if needed, physicians were free to implement clinical actions remotely or schedule in-office visits.
The objectives of this analysis were:
- to describe the implementation of the HeartLogic algorithm in a protocol for the remote monitoring of HF patients
- to evaluate the approach to diuretic dosing and timing of the intervention in patients with device alerts.
Results:
From December 2017 to July 2020 HeartLogic was activated in 229 patients in 8 Italian centers.
During a median follow-up of 17 months, 242 alerts (0.8 alerts/patient-year) were reported in 123 patients.
105 (44%) alerts were not followed by HF therapy (nonactionable, unexplained, or associated with non‐HF‐related conditions)
137 (56%) alerts triggered clinical actions to treat HF
- 56 decongestive treatment augmentations only (increase in the equivalent dose of diuretics or switch to a more bioavailable diuretic)
- 81 mixed interventions
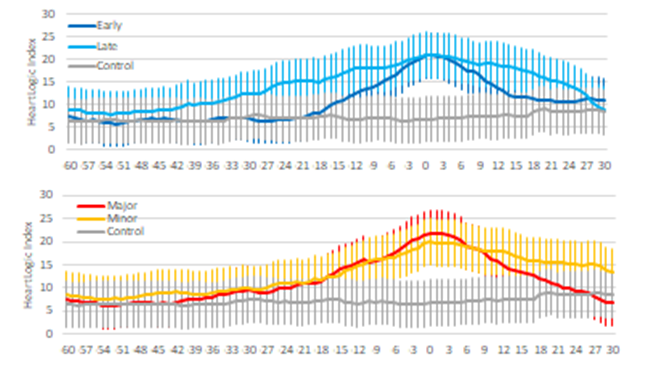
The analysis of HeatLogic trends surrounding the decongestive treatment adjustment, showed that:
- The alert status resolved more quickly when decongestive therapies were timely (< 2 weeks) and major (>2 times the daily dose), as observed in Figure 1.
- The duration of “in-alert” status was shorter when decongestive therapies were timely in comparison with late changes (28 days versus 62 days, p<0.001). Major and minor diuretic augmentations resulted in comparable alerts durations.
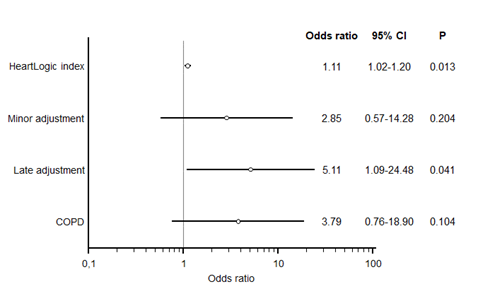
- The need of hospitalization for further treatments to resolve the alert condition was associated with higher HeartLogic index values on the day of the diuretics and with late interventions (Fig. 2)
EHRA and HRS Congresses
Two important congresses took place in April:
- EHRA: Copenhagen & Online, 3 – 5 April
- HRS: San Francisco, April 29 – May 1
During these meetings some new findings about performance of HeartLogic have been presented, and below you can find the details.
EHRA 2022
Four HeartLogic posters have been presented during the Congress of European Hear Rhythm Association

Santobuono et al, presented this analysis in order to investigate the performance of HeartLogic that has been poorly investigated in non-CRT patients, as well as in relation to the presence of comorbidities.
Results:
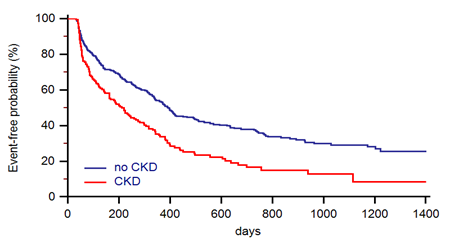
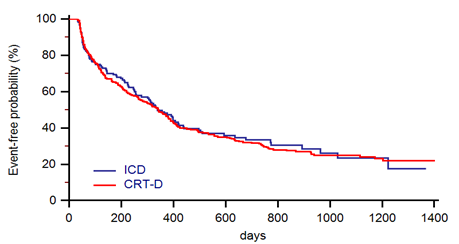
The HeartLogic feature was activated in 568 ICD patients (410 with CRT) from 26 centers. During a median follow-up of 25 months 1200 HeartLogic alerts (0.71 alert/pt-year) occurred in 370 patients.
HeartLogic alerts, while alerts were not associated with CRT vs. non-CRT device implantation (Fig. 1c)
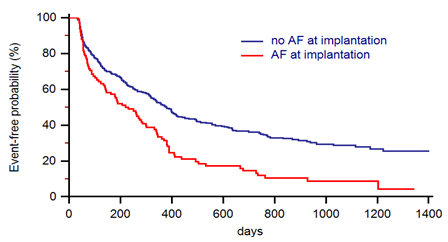
- The incidence rate ratios of clinical events (cardiovascular hospitalization or death) in the IN alert state Vs in the OUT of alert state ranged from 9.72 to 14.45 (all p>0.001) in all group of patients: CRT/non-CRT, AF/non-AF, CKD/non-CKD (Table 1))
- The time IN the HeartLogic alert state >13% was associated with the occurrence of clinical events (HR: 2.54, 95%CI:1.61-4.01, p<0.001).
Conclusions:
This analysis seems to confirm that patients with AF and CKD are more exposed to experience HeartLogic alerts. HeartLogic algorithm identifies patients during periods of increased risk of clinical events regardless of the type of device, AF or CKD
The effect of sacubitril/valsartan on device detected heart failure status
F Giordano 1 , L Striuli 1 , AV Pollina 1 , N Mumoli 1 , D Spaziani 1
Giordano et al, from G. Fornaroli Hospital, Magenta (Italy), presented an interesting analysis evaluating the effect of Sacubitril/Valsartan on HeartLogic algorithm in HFrEF patients with an implantable cardioverter-defibrillator (ICD). The secondary objective was to analysis the effect of Sacubitril/Valsartan therapy on ventricular arrhythmias events.
Results:
36 ICD patients (83% male, age 69±6) with HFrEF (LVEF ≤ 35%) and at least an HL alert, were consecutively enrolled and treated with Sacubitril/Valsartan on top of standard therapy. At 12 months follow-up, irrespective of Sacubitril/Valsartan dose: HeartLogic alerts were significantly reduced (HL 38 vs 24; p=0,024) NT-proBNP serum levels were significantly reduced (2358 vs 1134 pg/mL; p=0,019) Both sustained and non-sustained ventricular tachycardia episodes decreased (3 vs 0.7; p =0,05 and 15.7 vs 2.2; p=0,04)
Conclusions:
The administration of Sacubitril/Valsartan effectively reduced HeartLogic index and NT-proBNP values supporting the favorable impact of this drug in HFrEF patients. The results confirm the reliability of HeartLogic algorithm for heart failure management. Thus, an alert-based follow-up approach can be used for therapy optimization in this population.
During Heart Rhythm Society Congress three posters
on HeartLogic have been presented.
For details about these posters, please refer to the previous EHRA content.
Implantable Defibrillator-detected Heart Failure Status Predicts Atrial Fibrillation Occurrence
M. Bertini, V.Tavoletta, A. Giano, L. Caló, L. Santini, G. Savarese, A. Dello Russo, V. E. Santobuono, M. Viscusi, C. Lavalle, C. Amellone, D. Pecora, S. Valsecchi, F.Vitali.
Decongestive Treatment Adjustments In Heart Failure Patients Remotely Monitored With A Multiparametric ICD Algorithm
F. Guerra, A. D'Onofrio, E. de Ruvo, M. Manzo, L. Santini, G. Giubilato, C. La Greca, B. Petracci, G. Stronati, V. Bianchi, A. Martino, F. Franculli, P. Compagnucci, S. Valsecchi, A.Dello Russo.
Sacubitril/Valsartan: Effects On Device Detected Ventricular Arrhythmias And On Device Based Heart Failure Status
F. Giordano, L. Striuli, A. V. Pollina, N. Mumoli, D. Spaziani.