Dear HeartLogic™ users,
Welcome to this new issue of the HeartLogic Newsletter.
We have the opportunity to share with you two interesting publications focused on HeartLogic™ and Atrial Fibrillation: the first one comes from the Italian HeartLogic Independent Registry, while the second one is an analysis from MultiSENSE Study.
A new case of the month, about HeartLogic and Atrial Fibrillation, is included in this newsletter.
HeartLogic™ predicts Atrial Fibrillation occurrence
An analysis from Italian HeartLogic Independent Registry has been performed by Dr. Bertini
(S. Anna Hospital, Ferrara, Italy) and recently published on Heart Rhythm Journal1
Implantable defibrillator-detected heart failure status predicts atrial fibrillation occurrence
As known, atrial fibrillation (AF) is a common comorbidity in heart failure (HF) patients, and it is associated with a significantly increased risk of mortality, morbidity and HF progression. Modern device diagnostics provide detailed information about HF status (HeartLogic), concurrent with atrial of high-rate events (AHRE) as a surrogate of AF on a daily basis.
Objectives and Methods:
- To investigate the association between the HeartLogic Index values and the incidence of AHRE during the follow-up period
- To evaluate the performance of the HeartLogic Index in detecting follow-up periods of significantly increased AHRE risk
From December 2017 to June 2021, HeartLogic was activated in 568 patients (ICD and CRT-D) in 26 Italian centers. Patients were followed according to the standard practice of the centers: remote monitoring checks, phone contacts at the time of HeartLogic alerts and, if needed, clinical actions as per center practice.
Results:
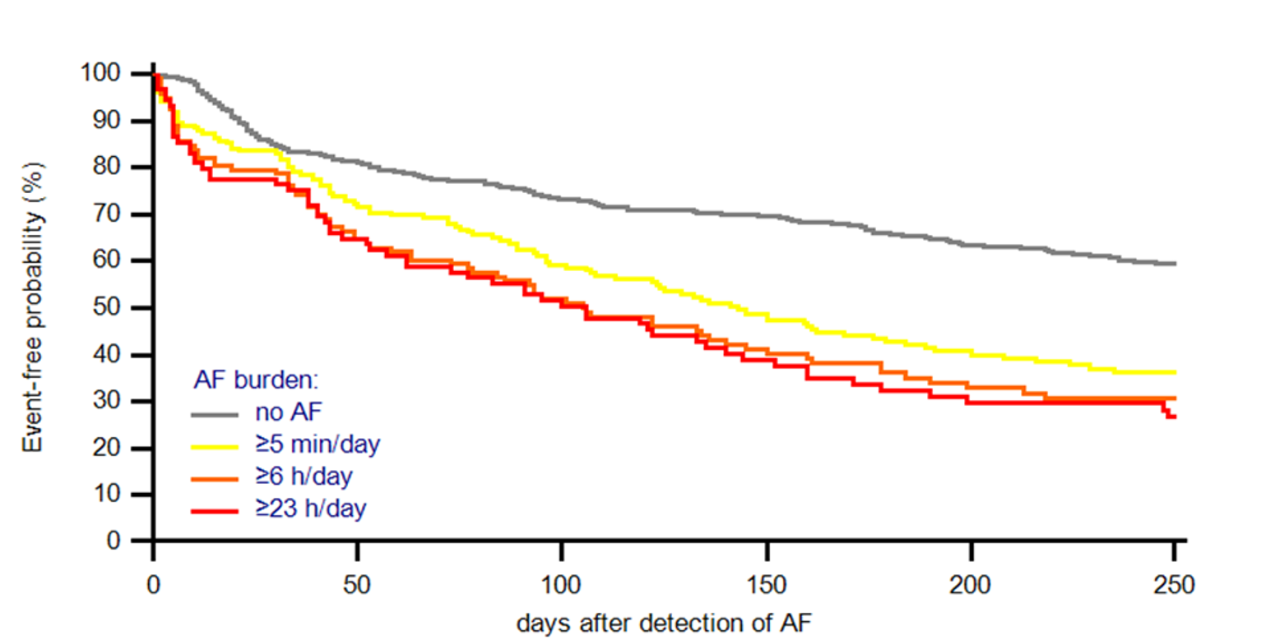
During a median follow-up of 25 months [25th-75th percentile: 15-35] the HeartLogic index crossed the threshold 1200 times (0.71 alerts/patient-year) and the AF burden observed was:
- ≥5 minutes/day in 32% of pts
- ≥6 hours/day in 21% of pts
- ≥23 hours/day in 16% of pts
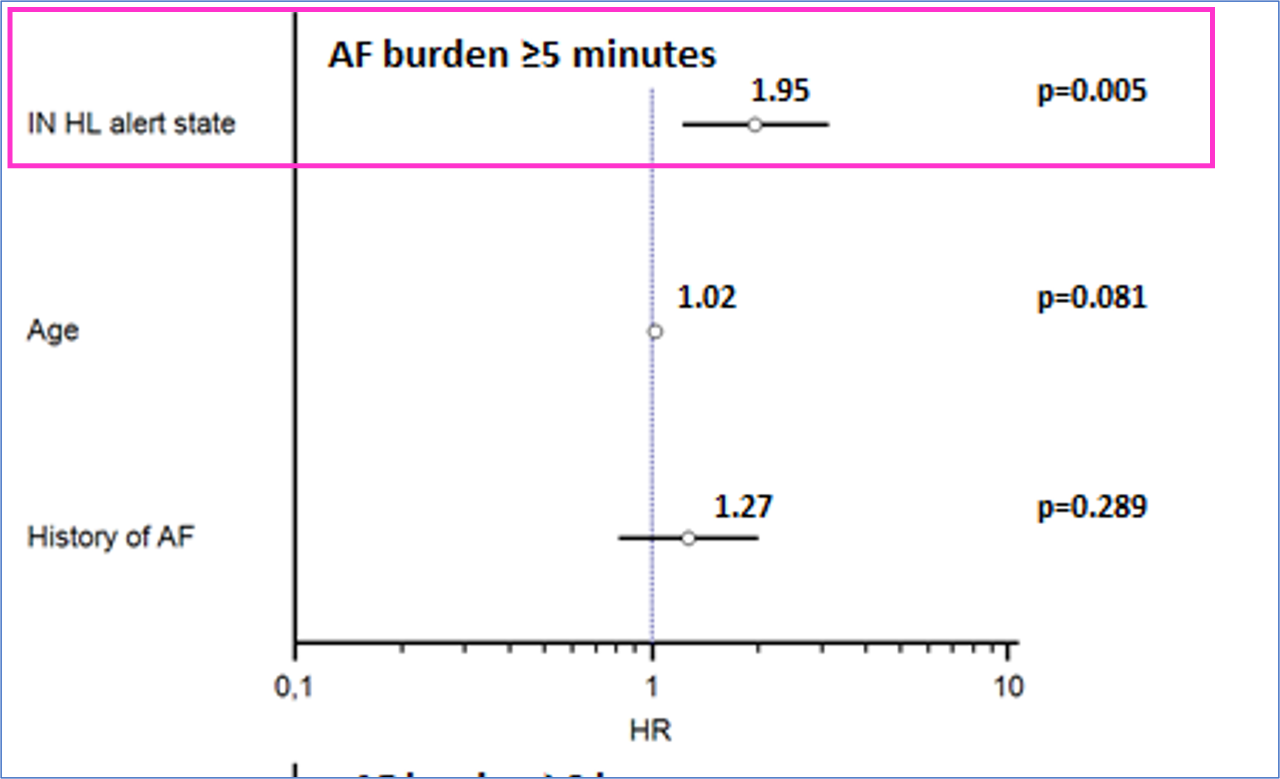
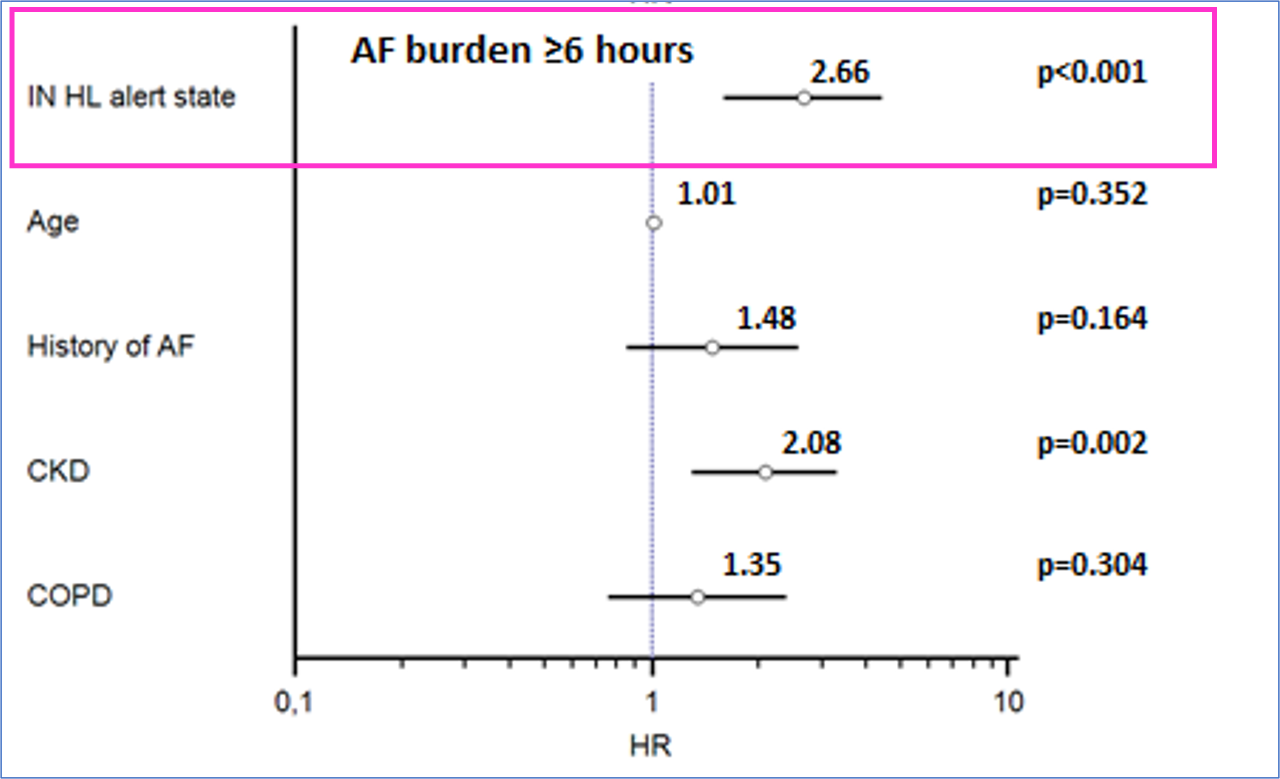
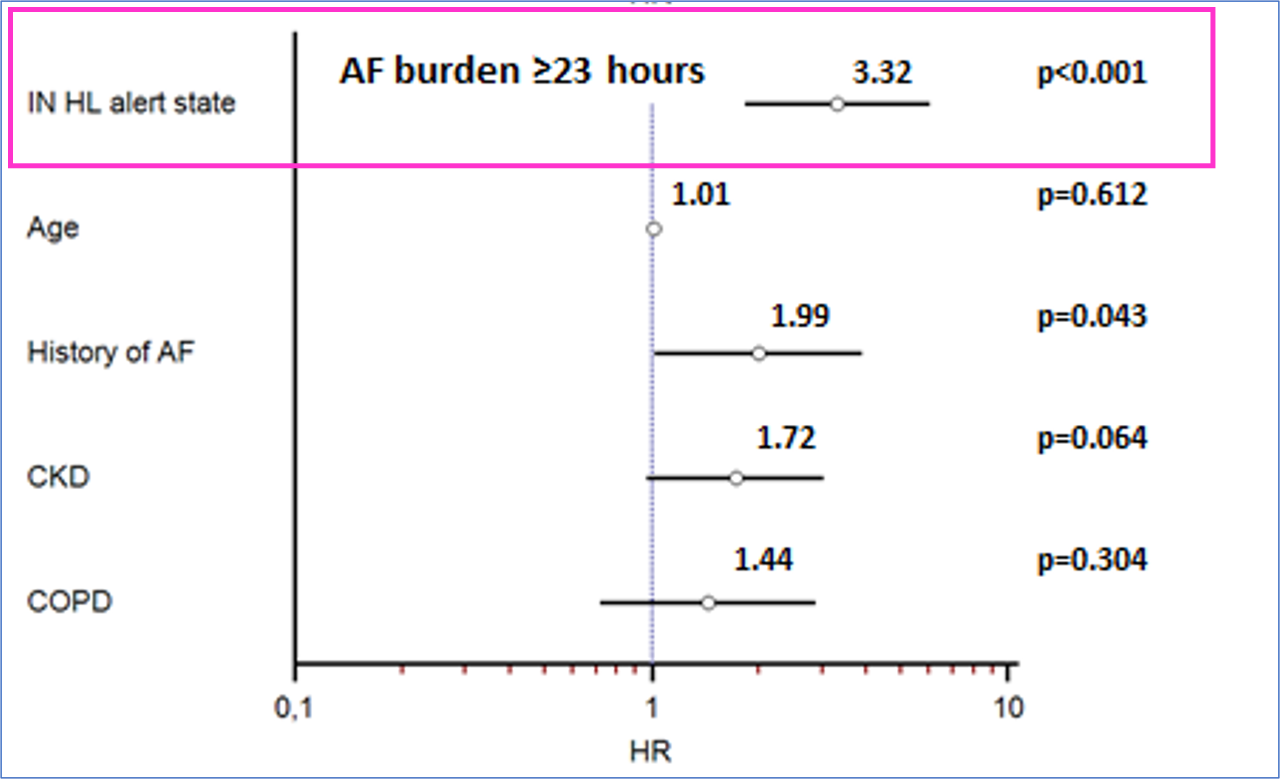
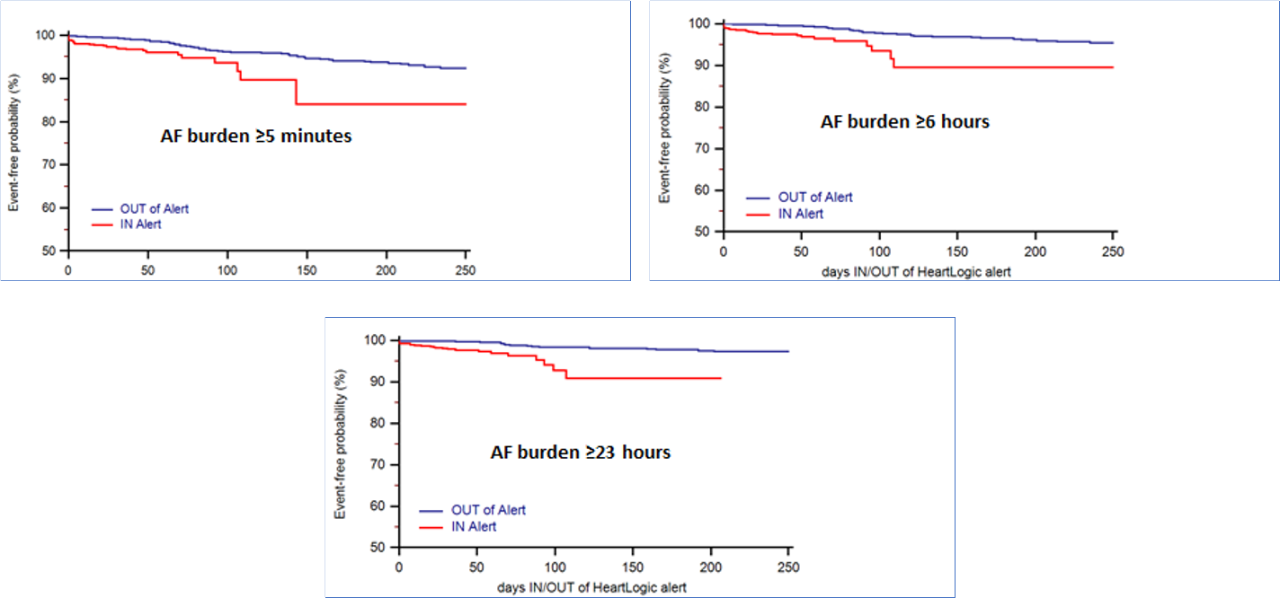
state showed that the intervals of time defined as periods of increased risk of HF also allow risk stratification of AF according to various thresholds of daily burden (Figure 2)
Conclusions:
- Patients who experienced at least one ICD-diagnosed HF event were those at greatest risk of having AHRE occurrence, according to various thresholds of daily AF burden.
- The study demonstrated the ability of HeartLogic to dynamically stratify patients during follow-up: the weekly IN-alert state identified patients who were from two- to more than three-fold more likely to experience an AHRE episode.
- The detection of AHRE was significantly associated with subsequent HeartLogic alerts (as surrogate of HF decompensation)
- A robust association between the HeartLogic alert state and AF was observed, and this association was even stronger when the AF burden was higher
MultiSENSE Analysis
Another interesting analysis from the MultiSENSE Study has been recently published by Prof. Capucci on JACC: Clinical Electrophysiology Journal2
Temporal Association of Atrial Fibrillation With Cardiac Implanted Electronic Device Detected Heart Failure Status
Heart Failure (HF) is known to predispose patients to AF via numerous mechanisms and history of AF (or new onset of AF) has been linked to an increased risk of HF hospitalization. However, it is not always clear if HF triggers AF or vice-versa.
Objectives and Methods:
This analysis, from MultiSENSE study, sought to investigate the temporal association between changes in physiologic sensors, AF burden, and clinical HF.
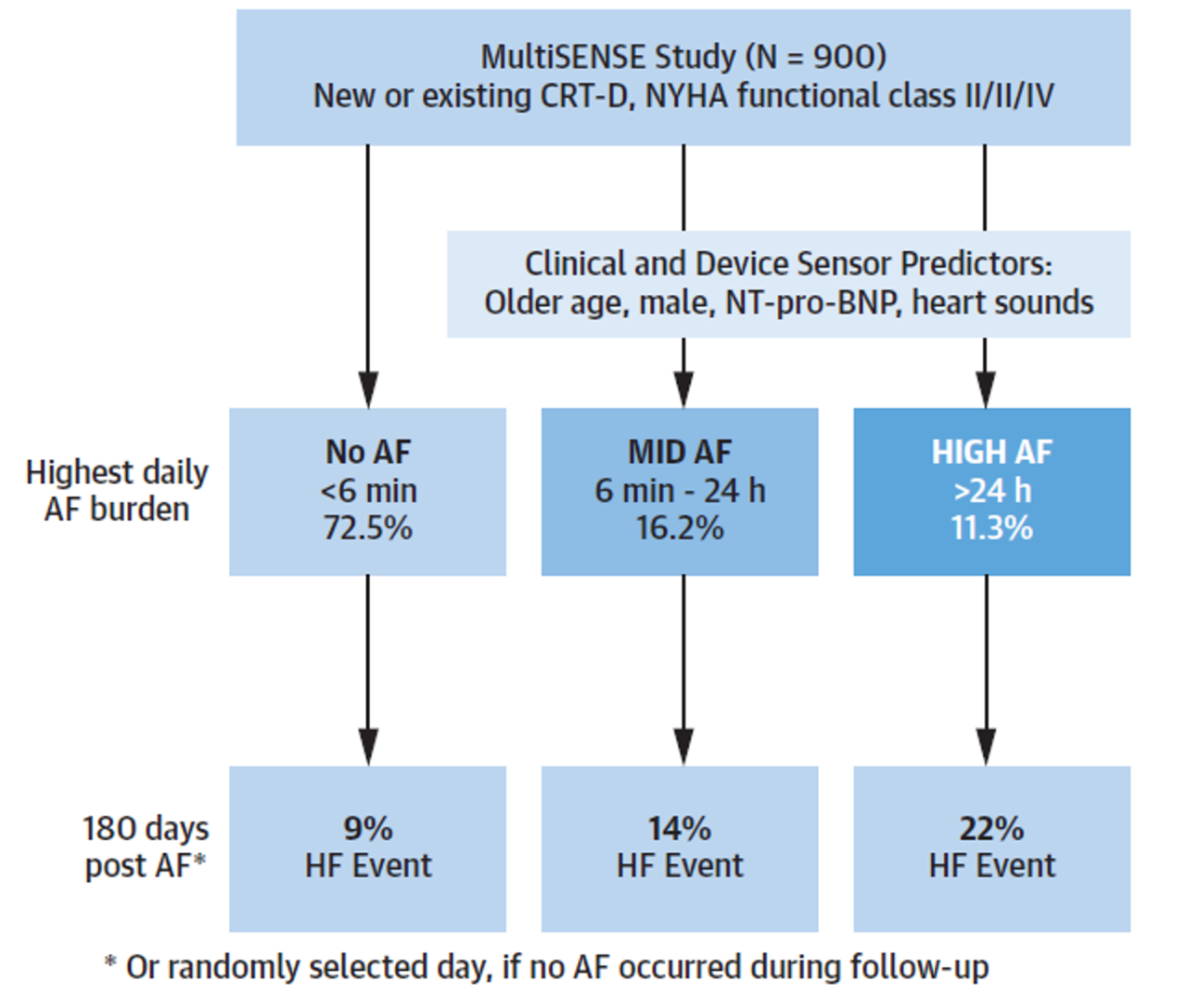
Patients were grouped according to their longest daily AF burden: HIGH AF (at least 24 hours of AF), MID AF (between 6 minutes and 24 hours) and NO AF (less than 6 minutes). The adjudication of HF events was performed by a Clinical Events Committee (CEC). Sensor data were aligned to the first qualifying AF event or a randomly selected day for patients in the NO AF group.
Results:
Among 900 patients enrolled in MultiSENSE study, 869 had device-measured AF data available during the median follow-up of 393 days (25th -75th percentile: 387- 399 days). Figure 1 shows the distribution of patients among the 3 AF groups and heart failure incidence after atrial fibrillation.
In the multivariable, time-dependent regression analysis, high AF burden was associated with twice the risk of having an HF event (HR: 1.96; 95% CI: 1.03-3.74; P = 0.041)
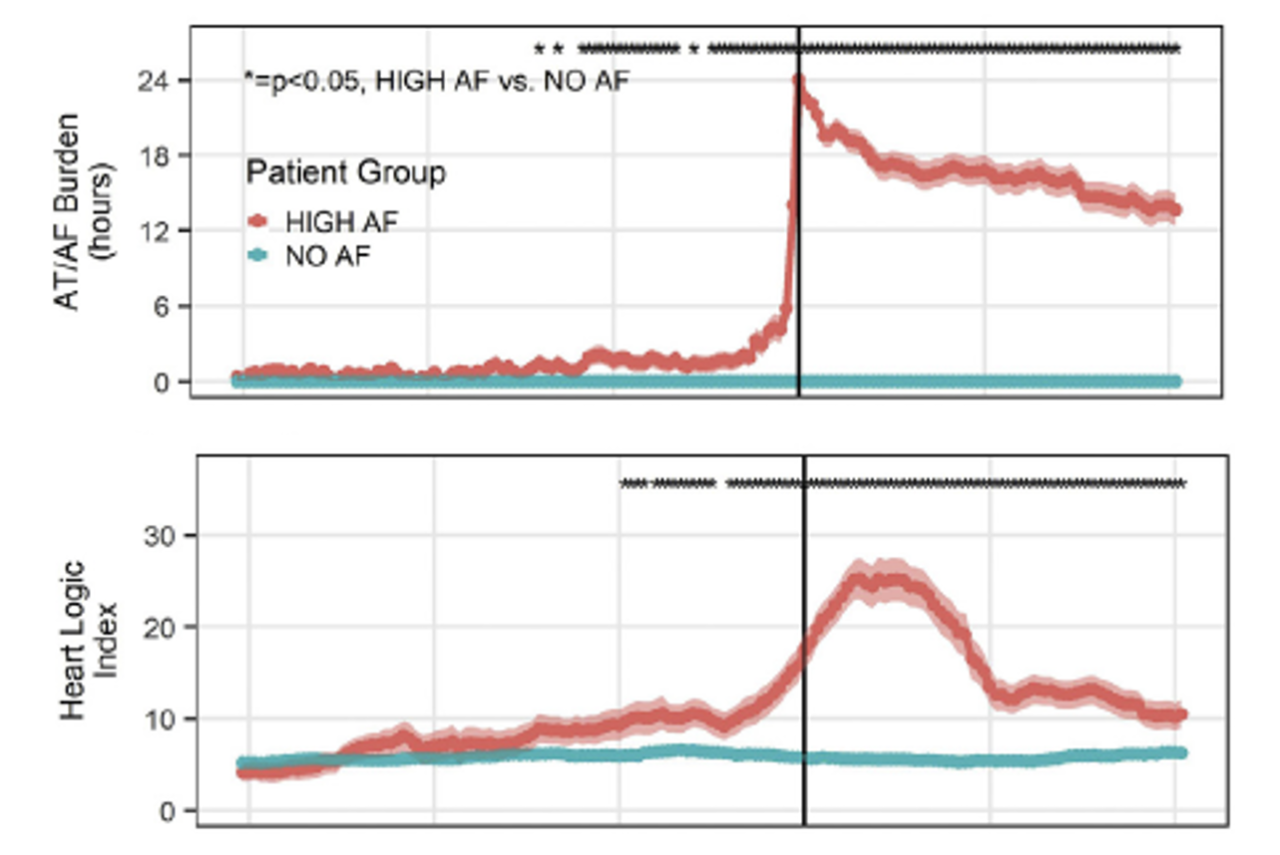
Figure 2 illustrates the temporal evolution of HeartLogic (B) index in the HIGH AF PATIENTS aligned with respect to the first day of 24-hour AF, and IN patients in the NO AF group aligned with respect to a randomly selected day (A).
The analysis of device measured sensors changes indicated:
- a significant worsening of HF status preceding new incidence of AF
- AF onset significantly changed multiple physiologic sensors, including the HeartLogic index
Across the 3 AF groups, the change in HeartLogic index was significantly different (NO AF: Δ = 0.34 ± 0.3, MID AF: Δ = 2.82 ± 1.34, HIGH AF: Δ = 9.75 ± 1.74; P < 0.001).
Conclusions:
- Worsening of HF status, as indicated by device-based sensors, preceded AF onset
- HF status worsened further after AF with an increased risk of HF acute events following AF.
These findings suggest the bidirectional interaction between AF and HF and also the role of progressive HF worsening as a possible cause of AF that further impairs cardiac function.
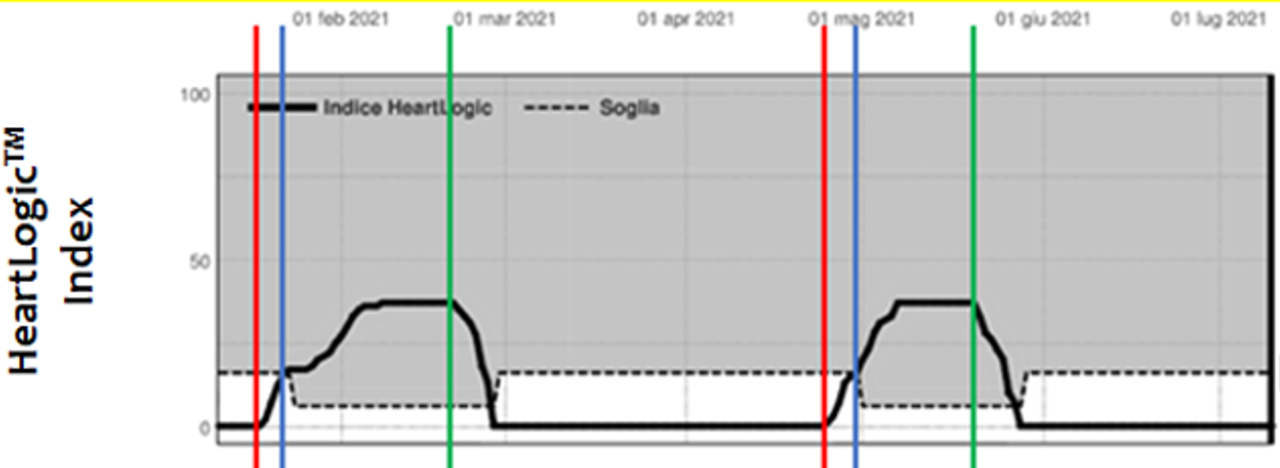
Case of the month
A 72-year old man with post-ischemic dilated cardiomyopathy, hypertension, dyslipidemia and paroxysmal atrial fibrillation underwent a VIGILANT™ EL dual-chamber ICD implantation in December 2019. The patient was enrolled in LATITUDE™ remote monitoring system and HeartLogic™ diagnostic algorithm was activated...