Dear HeartLogic™ users,
In this issue we are pleased to share with you content about HeartLogic presented during the European Heart Rhythm Association (EHRA) Congress - which took place few weeks ago: a live presentation and two posters.
Furthermore, it is our pleasure to share with you an interesting analysis from the MultiSENSE Study published by Dr. Cao on International Journal of Cardiology.
In this issue you can also find a new case of the month.
EHRA 2021 Congress
EHRA 2021 took place remotely between 23 and 25 April. Devices, diagnostic tools and drug therapy were introduced during the Congress.
We would like to share with you a live presentation and two posters. All of them focus on the risk stratification made by HeartLogic and on HF patient management during COVID-19 pandemic.
Live Presentation
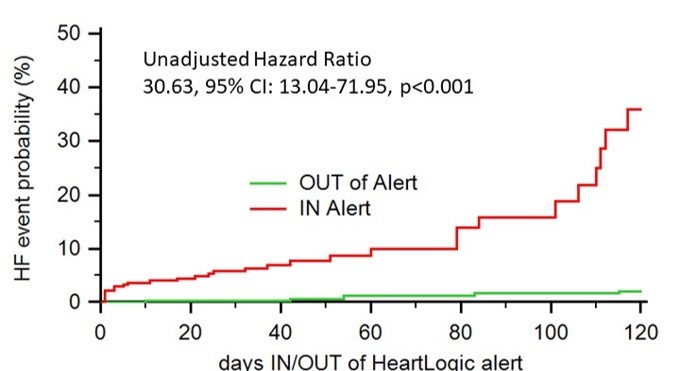
During the live presentation session “News about remote monitoring and pacing”, Dr De Ruvo (Policlinico Casilino – Rome , Italy) presented an analysis - coming from the Italian HeartLogic Registry - about the risk stratification ability of HeartLogic in clinical practice.
A multiparametric ICD algorithm for heart failure risk stratification and management: an analysis in clinical practice
The analysis was performed on 366 patients. During a median follow-up period of 11 months, 36 HF hospitalizations and 8 deaths for HF were observed (0.12 events/pts-year)
This study demonstrated
- The ability of the HeartLogic algorithm to identify patients during periods of significantly increased risk of HF events in clinical practice.
- A proactive strategy in response to alerts may have a positive clinical impact.
- The use of HeartLogic does not generate a higher workload in the centers and may enable an efficient use of healthcare resources for the management of HF patients.
Poster Session

This poster examined how the HeartLogic performance, related to the changes in patients’ behaviour, impacted on HF decompensation and possible consequences of home confinement caused by the COVID-19 pandemic.349 devices were analyzed , the observation period was divided in:
- Pre-Lockdown: 1-11 weeks
- Lockdown: 12-20 weeks
- Post-lockdown: 21-29 weeks
Analysis of alerts occurred:
The average duration of the in-alert status was similar in all the 3 study phases, as well as the maximum value of the index.
| Alerts, n | Rate [95% CI], Alerts/100pt-weeks | Alerts with actions | Remote management | |
| Pre-lockdown | 35 | 0.91 [0.64-1.27] | 11 (31%) | 31 (89%) |
| Lockdown | 49 | 1.56 [1.15-2.06] | 11 (22%) | 44 (90%) |
| After-lockdown | 43 | 1.37 [0.99-1.84] | 12 (28%) | 38 (88%) |
Analysis of Latitude Trends
After “stay at home” orders:
- There was a significant drop in the activity level that persisted until week 19.
- There was no difference in the other contributing sensors.
The composite HeartLogic index significantly increased at the end of Lockdown (from week 20), and the increase in the average index remained significant until week 28 in the Post-Lockdown phase.
In conclusion:
- Despite all the efforts to preserve the quality of care in HF patients during the home confinement, behavioral changes and the possibility of discontinuous treatments may have a negative effect on patients’ outcome.
- The system was sensitive to the behavioral changes occurred during the lockdown, i.e. decrease in activity. However, the home confinement had no impact on the other sensors.
- The HeartLogic multisensor platform can improve the quality of care in HF patients with ICDs, especially in periods of prolonged social distancing ensuring a constant monitoring of HF status.
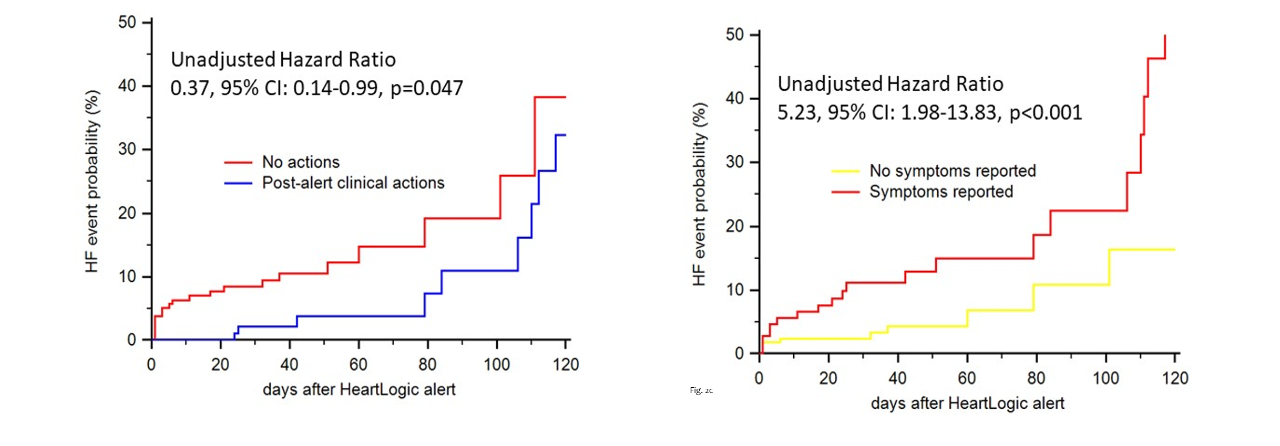
49 HF patients were enrolled and there was a comparison between patients with HeartLogic alert (Group A) and patients without HeartLogic alerts (Group B) during COVID-19 pandemic.
- Group A had more unstable HF events with 10/21 (47.6%) having their first HeartLogic alert during the pandemic.
- Multiple HeartLogic alerts, longer period in HeartLogic alert, patients with ischemic aetiology of HF were higher in Group A.
In conclusion:
- Patients with ischaemic etiology of HF and with more HeartLogic alerts prior to the pandemic did worse.
- First HeartLogic alerts, multiple alerts and longer duration of alerts in Group A suggest a lack of access to adequate HF services during the COVID-19 pandemic.
From Multisense Study
An interesting publication from the MultiSENSE Study has been recently published by Dr. Cao on the International Journal of Cardiology.
Small decreases in biventricular pacing percentages are associated with multiple metrics of worsening heart failure as measured from a cardiac resynchronization therapy defibrillator
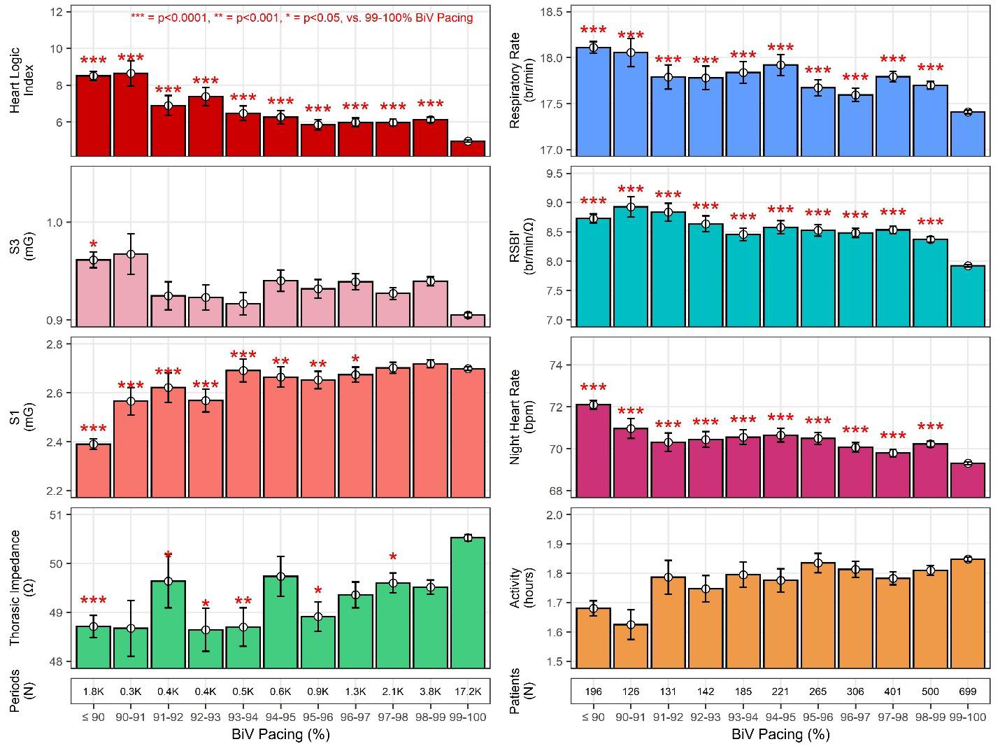
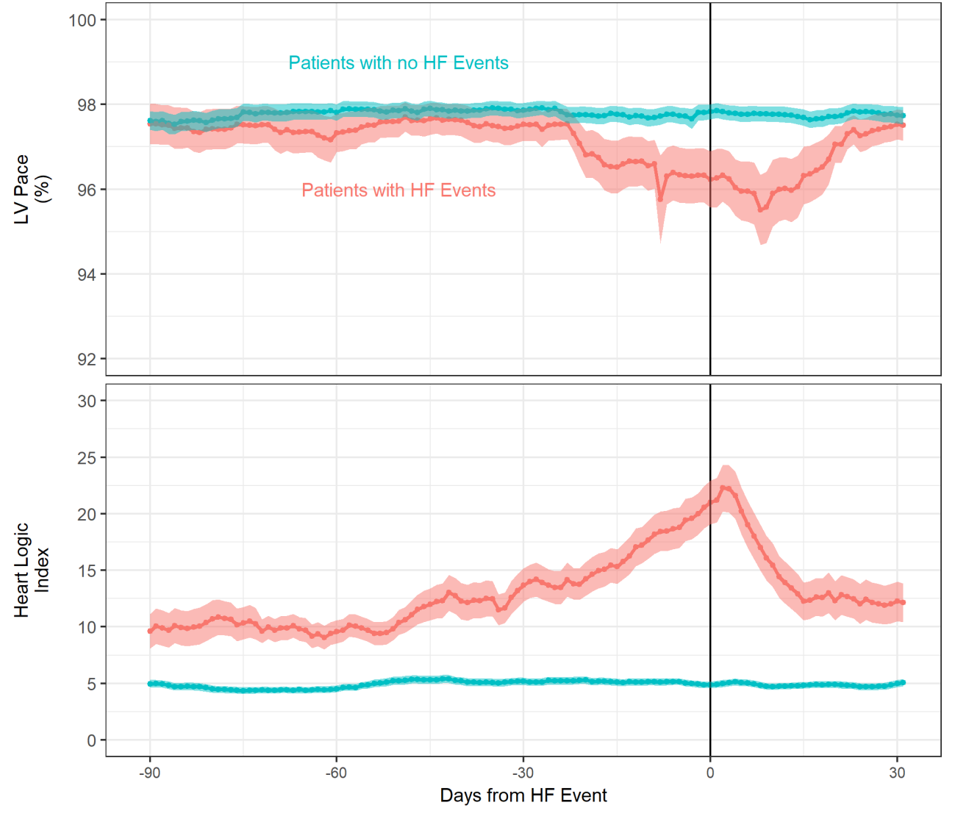
This analysis evaluated whether small incremental decreases in BiV pacing percentages were associated with worse measures, related to Heart Failure physiology using the composite HeartLogic Index, individual HF sensors, and the time before a HF event as indicative of worsening HF and after the HF event as indicative of return towards baseline.
Sensor data were obtained from 900 ambulatory HF patients with implanted CRT devices and the percent of cardiac cycles with BiV pacing was assessed for periods (median = 7.3 days) between data downloads (median = 55 periods/patient).Optimal percentage of BiV pacing was defined as greater than or equal to 98% based on the 2015 HRS/EHRA/APHRS/SOLAEC Expert consensus statement on optimal implantable cardioverter-defibrillator programming and testing (IIa recommendation).
Physiological Sensors and BiV Pacing Percentage
Worsening sensor signals, related to HF physiology, were found with progressively lower pacing percentages (Fig. 3).
IN the HeartLogic alert status, using the nominal alert threshold of 16, the probability of optimal BiV pacing (≥98%) was lower than when OUT of the HeartLogic alert status, for a given subject (OR: 0.655; 95% CI: 0.626 - 0.686; p<0.0001).
The matched-pair analysis using signal statistics during optimal LV pacing (>98%) versus period with sub-optimal LV pacingshowed significantly elevated respiration rate, rapid shallow breathing index (RSBI), night-time heart rate and HeartLogic index value.
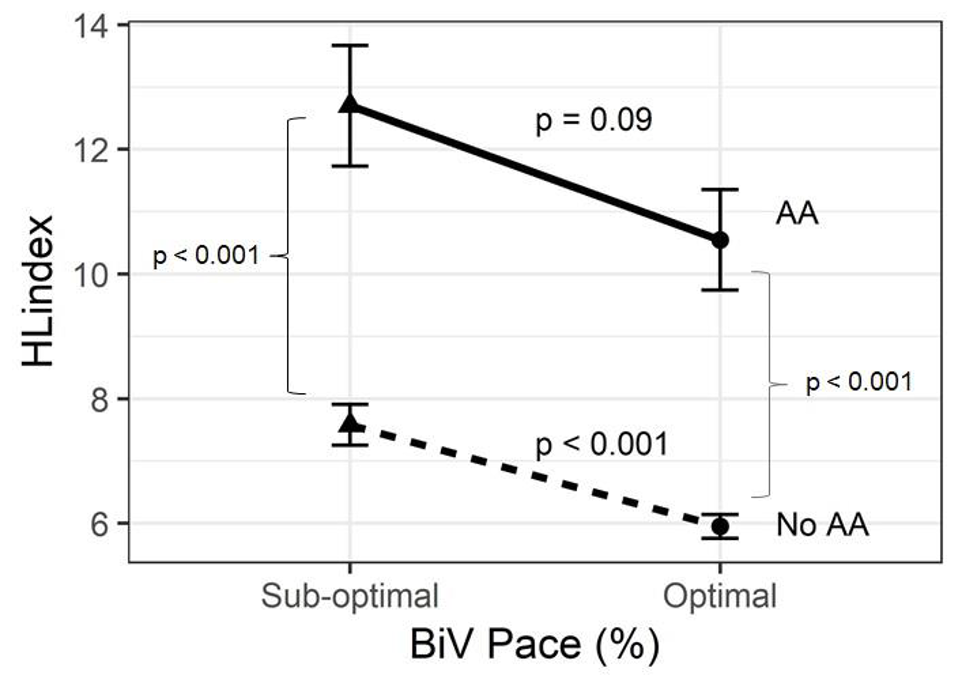
Biv pacing and arrhythmias
Subjects with constant optimal pacing (≥98% BiV) were less likely to have a:
- history of Atrial Fibrillation (22% vs. 34%, p<0.001).
- period of Atrial Arrhythmias (19% vs. 37%, p<0.0001).
- lower mean daily Atrial Aarrhythmias burden (0.51 ± 0.15 hours vs. 1.56 ± 0.21 hours, test for equality of proportions p < 0.0001).
Atrial Arrhythmias (AA) were associated with an elevation of the HeartLogic Index (Fig. 4)
Conclusions:
- Authors provided observational evidence that lower BiV pacing percent can lead to multiple markers of worsening HF and patients with worsening HF as evidenced by entering HeartLogic alert are more likely to have suboptimal BiV pacing.
- These observations support the recommendation to maximize BiV percent pacing not only to prevent morbidity and mortality events, but also to improve the HF condition.
- This is the first demonstration of worsening HF associated with lower BiV percent pacing using objective metrics from an entire cohort of HF patients
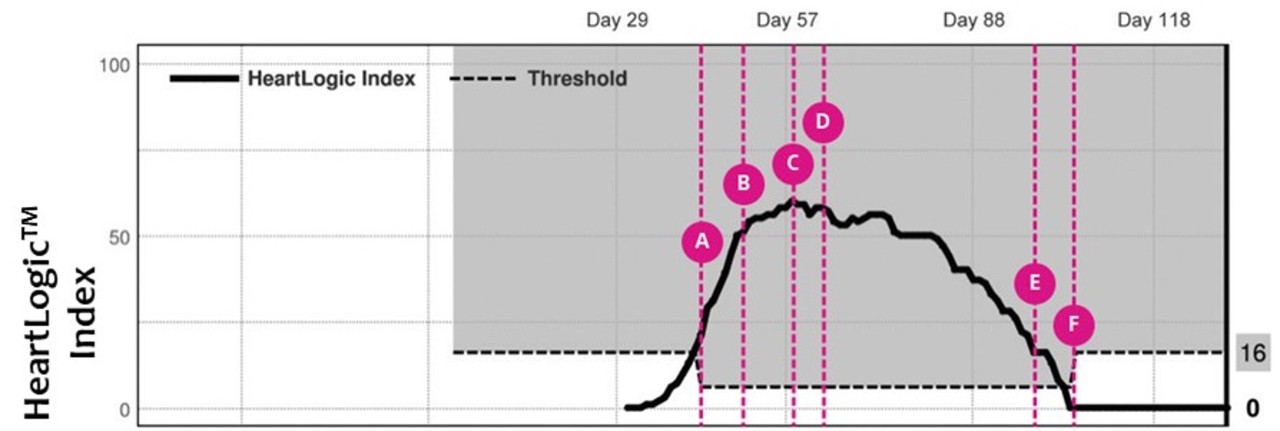
Case of the month
A 68 years old woman with dilated cardiomyopathy, severe mitral regurgitation and LBB presented in ER with symptoms of fatigue, dyspnea on exertion and shortness of breath. She underwent left and right heart catheterization due to severe Heart Failure.
The patient was admitted to the hospital for 25 days and a Vigilant CRT-D device was implanted.
During hospital stay the patient continued to have…