Dear HeartLogic™ users,
We are pleased to share with you a review of the most important clinical evidences about HeartLogic, published on Sensors Journal. In this review you could find suggestions about HeartLogic daily use in clinical practice and an overview of ongoing trials and future perspective.
In this issue you can also find a new case of the month.
Review of HeartLogic publications
A review of the most important publications about HeartLogic algorithm has been published on Sensors Journal by Dr. Feijen at al. from the University Medical Center of Leiden (Netherlands).
“Early Detection of Fluid Retention in Patients with Advanced Heart Failure: A Review of a Novel Multisensory Algorithm, HeartLogic™”
Introduction
In the last years different tools have been released in the market in order to anticipate and minimize the acute heart failure events, especially using remote monitoring of fluid retention in patients who have ICD devices.
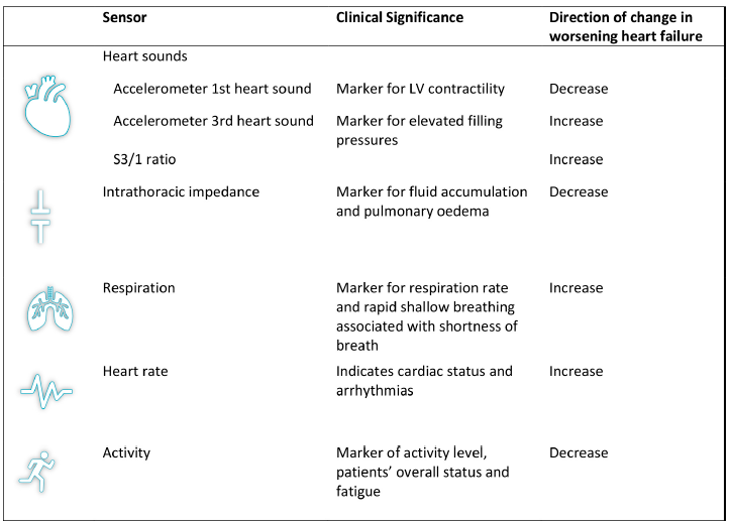
HeartLogic is a promising example of the novel multisensory approach. Data from multiple physiological sensors (heart sounds, respiration, thoracic impedance, heart rate and activity) are continuously collected by the device that combines them into one composite HeartLogic index.
If HeartLogic index increases and crosses the programmed threshold, an alert is notified to the center as the clinical status of the patient is worsening.
Evidence to Date
In this review, authors included all the most relevant publications and citations available up to last December about HeartLogic.
They picked the six studies below:
Authors | Study Design | # Patients | Primary Endpoint | Secondary Endoint |
Boehmer et al. | MultiSENSE Study | 974 | -Sensitivity: 70% -Specificity: 87.5% -Alert first proceeded the HF event a median 34 days. | Unexplained alerts rate: 1.47 alerts/pts-year |
Gardner et al. | MultiSENSE Study (Post-hoc analysis) | 900 | -IN alert state associated with 0.80 events/pts-year vs. OUT of alert with an event rate of 0.08 events/pts-year. (Event ratio IN/OUT 10.6.) | 50-fold risk of HF even when high NT-proBNP and IN alert vs. low NT-pro BNP and OUT alert state |
Capucci et al. | Italian Pilot (Retrospective analysis) | 67 | -0.99 alert/pt-year -Time IN ALERT state: 12% of observation period -Sensitivity: 100% | -Unexplained alerts rate: 0.41 alert/pt-year -Median early-warning time was 38 days in the case of hospitalizations and 12 days in the case of minor events of clinical deterioration of HF |
Calò et al. | Italian Pilot (heart sounds analysis) | 104 | - S3 detects a restrictive filling pattern sensitivity: 85%; specificity: 82%) - S1 detects LVEF < 35% (sensitivity: 28%; specificity: 88%) | More impairment of systolic and diastolic function was associated with more frequent signs of functional limitation and congestion. |
Santini et al. | Italian Pilot (prospective analysis) | 104 | -60% of alerts are clinically meaningful (associated with HF-related conditions) -Most frequent action triggered by an alert was the diuretic increase | High association between the alert state and the severity of HF: extremely low frequency of signs and symptoms reported during scheduled visit when the patient was out of the HeartLogic alert state. |
Mitter et al. | Retrospective case series | 38 | Observation of pre-COVID period Vs lockdown period: -drop in activity level and decrease in heart rate -no difference in median composite HeartLogic scores |
|
HeartLogic in Daily Clinical Practice
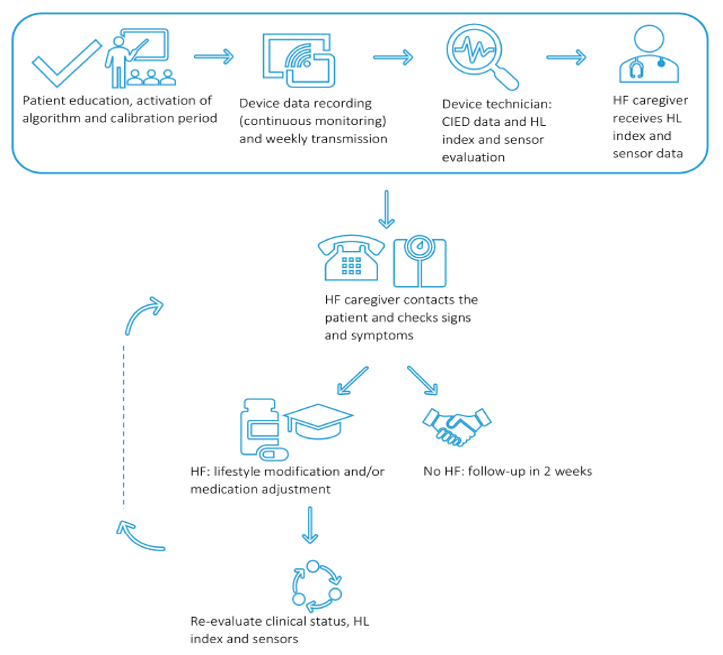
Roles and responsibilities of all healthcare professionals and the overall course of action should be well defined and standardized since the beginning.
In the case of a HeartLogic™ alert, the device technician analyses the CIED interrogation data and informs the heart failure specialist about the “in alert” status of the patient. The heart failure specialist contacts the patient in order to check potential signs and symptoms of fluid retention. In case of suspect of decompensated heart failure, the physician will manage the situation accordingly with lifestyle advice, medication adjustments and clinical evaluation. The effect of the above intervention will be evaluated by reassessment of the clinical condition of the patient and the HeartLogic™ index.
HeartLogic in Daily Clinical Practice
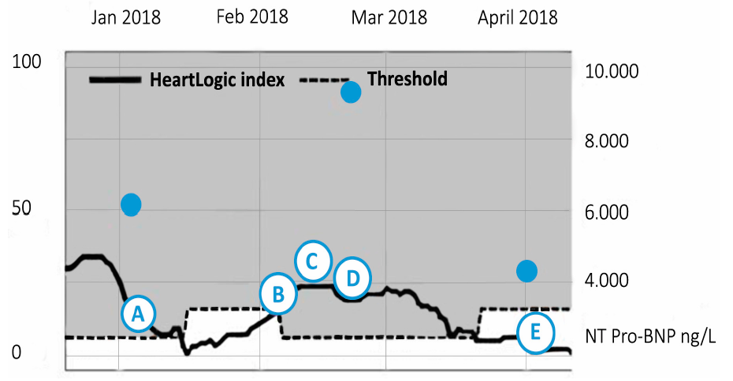
Physical examination showed elevated jugular venous pressure and mild ankle oedema and the pro-BNP level had increased to 9650 ng/L. The physician decided to increase the diuretic dosage. After these changes, HeartLogic index declined to 0, signs and symptoms of heart failure disappeared and the pro-BNP level declined to 4173ng/L.
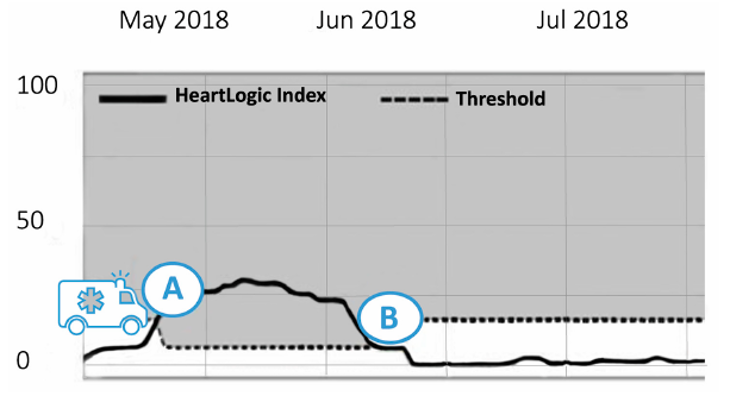
Case 2: HeartLogic™ Index as an Accurate Reflection of the Fluid (and not arrhythmia) Status
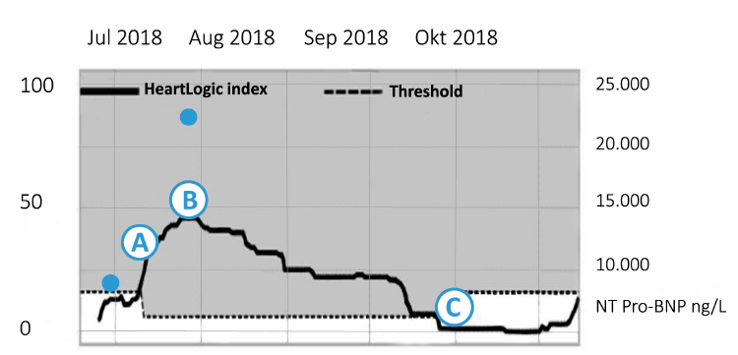
In April 2018 he was admitted with dyspnoea due to a symptomatic slow ventricular tachycardia terminated by antitachycardia pacing. The HeartLogic index was under the threshold and the echocardiographic evaluation revealed no signs of congestion or worsening of heart failure status.
On May 29th (point A) an HeartLogic alert was notified and, at phone contact, the patient reported a decrease in exercise capacity and weight increase (2 kilograms) in the last 4 days.
The diuretic therapy was increased just for three days: the patient’s weight returned to the target, his exercise capacity improved and after two weeks HeartLogic index decreased to 0.
Case 3: HeartLogic™ Index in a Complex Clinical Scenario of Decompensated Cardiorenal Function
A 64-year-old female patient with permanent atrial fibrillation, valves plasty and chronic kidney disease developed a cardiorenal syndrome and was hospitalized for heart failure. She underwent a CRT-D upgrading (from ICD for primary prevention of sudden cardiac death implanted in 2009) because intraventricular disorder and wide QRS.
Few weeks after, due to renal deterioration, she was started on hemodialysis twice a week.
Despite an increase in diuretic dosage, the fluid retention persisted and, after nephrologist consultation it was decided to extract extra fluid during each dialysis session.Subsequently, the HeartLogic index decreased and heart failure symptoms improved.
Ongoing Studies
- MANAGE-HF: Randomized study to evaluate the clinical efficacy of ICD remote monitoring of HF with or without HeartLogic.
- PREEMPT-HF: Prospective study focused on association between HeartLogic™ sensors and rehospitalization within 30 days after an index heart-failure-related hospitalization.
- Independent study by Dr. Treskes (recently published): HF hospitalizations comparison one year before and one year after HeartLogic activation.
- Independent French study: focused on annual HF hospitalizations rate and evaluation of HeartLogic index.
Future Perspective
In addition, it is clear the need of investigating whether mild symptoms or an alerts justify therapeutic adjustments.Another point that should be evaluated is the efficacy of the HeartLogicTM feature in specific patient groups: in particular in patients with advanced HF where traditional heart therapy are no longer effective or in specific patients with renal disease, LVAD, HFpEF,...
Case of the month
A 75 years old man with non-ischemic dilated cardiomyopathy and paroxysmal atrial fibrillation implanted with ICD for primary prevention of sudden cardiac death, was admitted for heart failure in August 2018. Left bundle branch block was diagnosed, and the patient underwent the upgrade to cardiac resynchronization therapy defibrillator (Resonate X4 CRT-D).
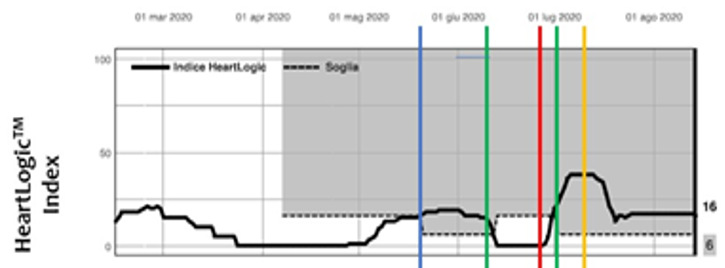
The HeartLogic algorithm was activated at the beginning of April 2020 and the patient remained stable for the following month.
On May 20th 2020 (blue line) HeartLogic triggered an alert and…