Dear HeartLogic™ users,
Welcome to the first 2021 issue of the HeartLogic Newsletter! We hope this year will be wonderful for yourself and your patients.
Let’s start 2021 with some interesting news about HeartLogic that we want to share with you:
- a case report on the performance of HeartLogic in a COVID-19 patient published in the Clinical Case Report Journal
- a new abstract presented at the American Heart Association Congress in November 2020
In this first issue, we are commenting these new clinical evidences and we are sharing a new patient case as well.
HeartLogic in Covid-19 patients:
a case series
New evidence about HeartLogic performace in patients affected by Covid-19 has been published by Dr. Shumway et al. (New England Heart and Vascular Institute, Catholic Medical Center, Manchester) on Journal of Cardiac Failure.
“Case Reports of Implantable Cardiac Device Physiologic Sensor Changes in Subjects with Coronavirus Disease-2019 Infection.”
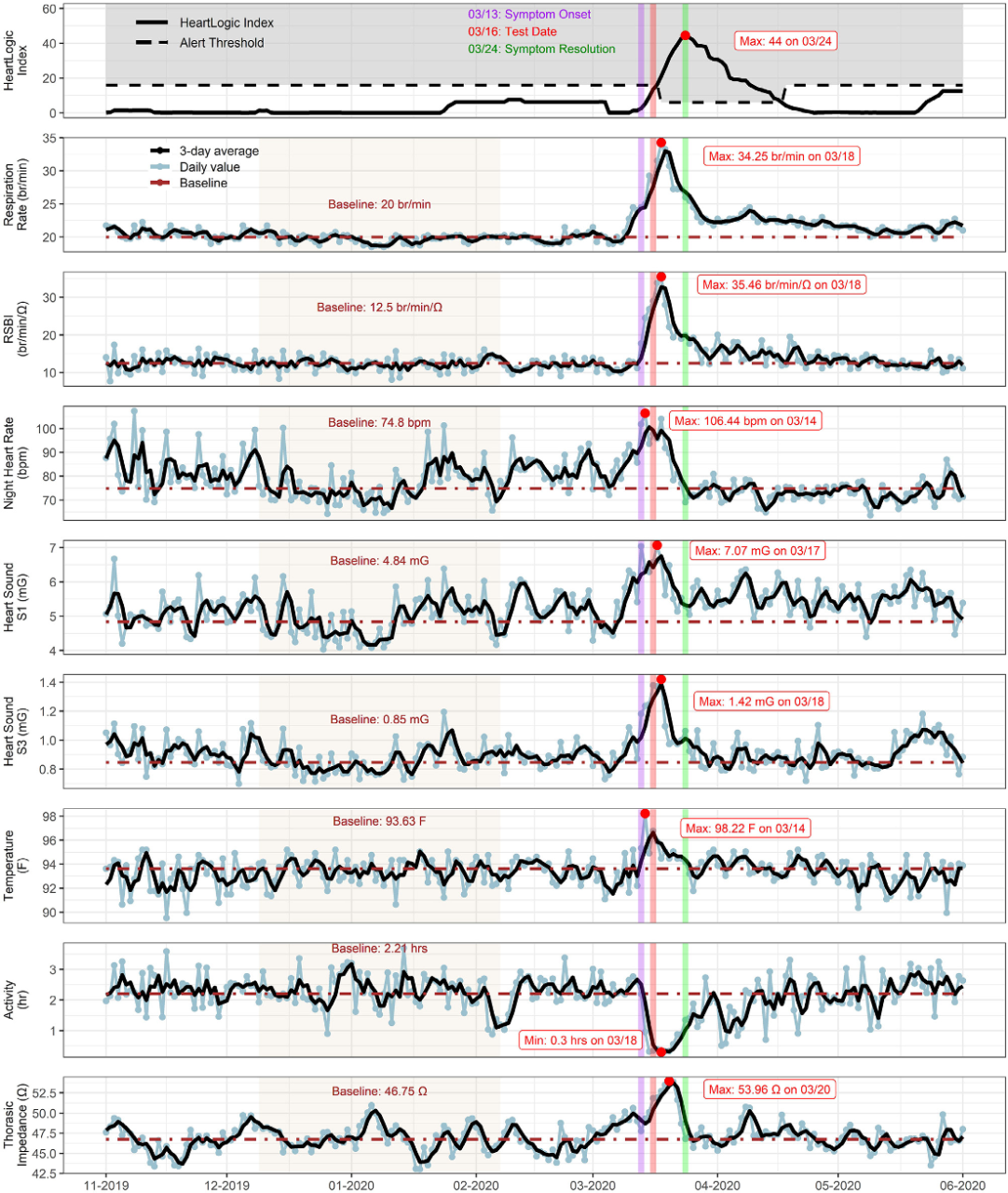
Authors reported three cases of patients with SARS-CoV-2 infection and the changes in HeartLogic physiological sensors trends.
The COVID-19 symptoms appeared at the same time of HeartLogic index increase: indeed, in the sensors report an increase in all physiological sensors, except activity level, has been observed.
Similarly, trends showed sensors restoration at the time of symptoms resolution.
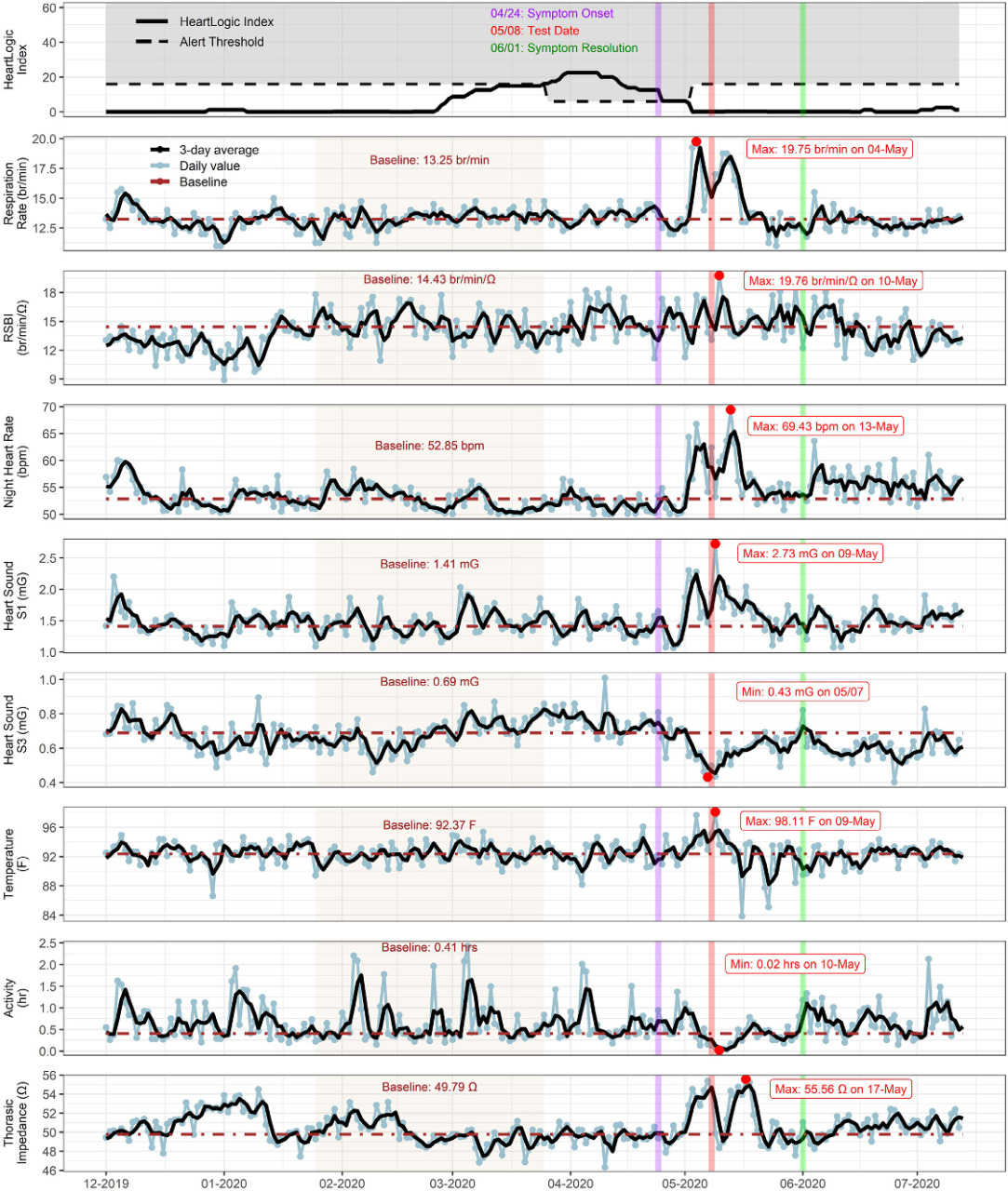
CASE 2 (Figure 2): A 67-year-old man with ischemic cardiomyopathy, atrial fibrillation/flutter, hypertension, hyperlipidemia, chronic kidney disease and diabetes was implanted with RESONATE ICD device.
From the end of April, the patient experienced different COVID-19 symptoms, but he was treated for SARS-CoV-2 infection only 10 days after, when he was hospitalized for hypoxia and respiratory distress and he was tested positive for COVID-19.
Respiratory sensor, heart rate, S1 and thoracic impedance showed two different peaks before and after hospitalization, while a decrease in S3 and activity level has been observed.
The values RSBI, S1 heart sound and thoracic impedance remained high for some weeks after discharge.
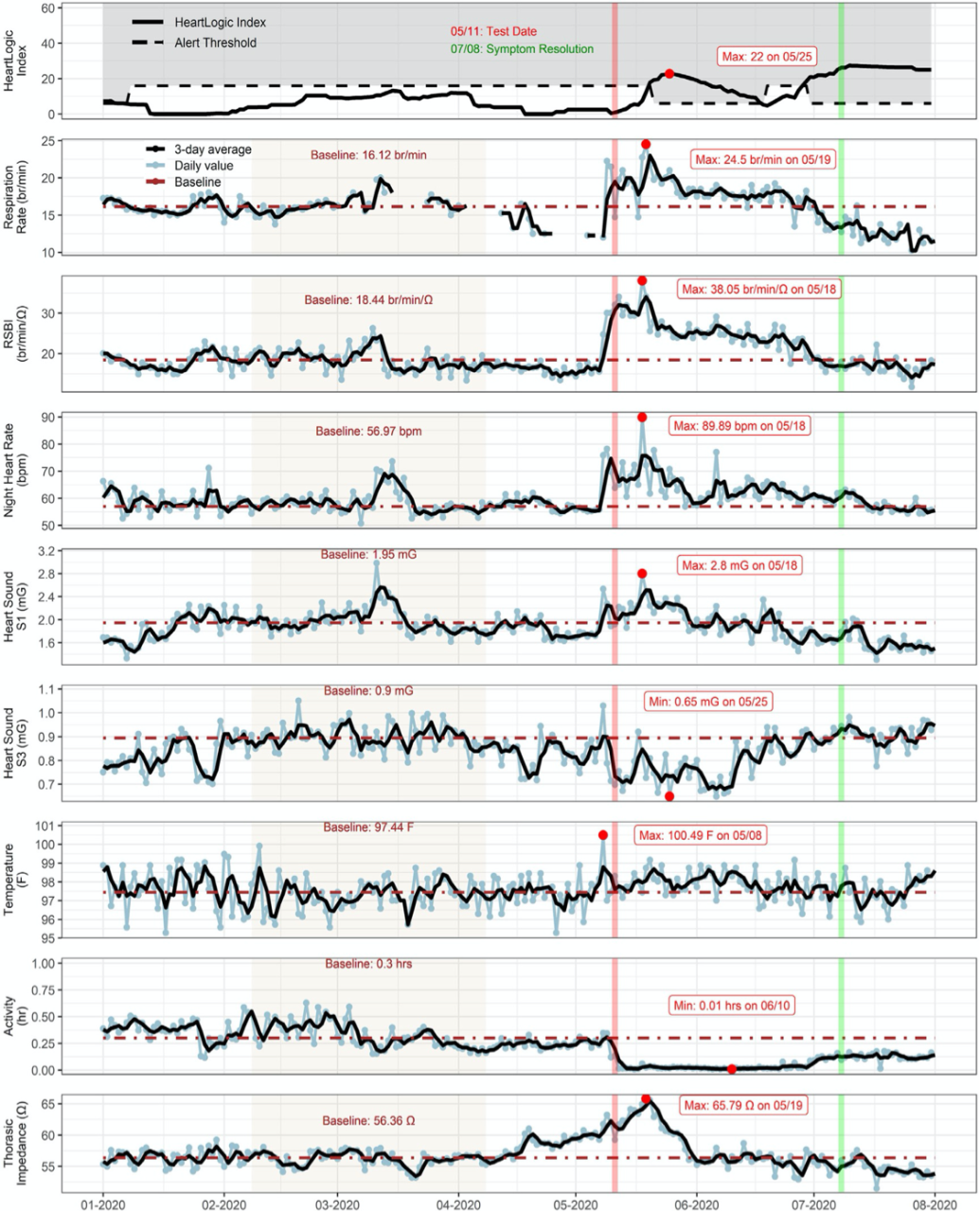
CASE 3 (Figure 3): A 78-year-old man with nonischemic cardiomyopathy, atrial fibrillation/flutter, hypertension, hyperlipidemia, chronic kidney disease and diabetes was implanted with RESONATE ICD device.
The patient was in long-term care facility and he was screened for COVID-19 as other patients had tested positive.The patient developed symptoms only after the positive test result and the first treatment for pneumonia.
As in the previous case, the respiratory sensor, heart rate, S1 and thoracic impedance increased during infection, while S3 and activity level showed a decrease.
Covid-19 and Heart Failure patient
Recently, the following paper about heart failure patient management during Covid-19 pandemic has been published on ESC Heart Failure journal:
“Beyond the stethoscope: managing ambulatory heart failure during the COVID-19 pandemic”
Dr. Oseran and his colleagues from Massachusetts General Hospital (Boston, USA) reviewed data on telemedicine and remote monitoring strategies to help physicians in heart failure patient management during Covid-19.As we well know the major Heart Failure and Cardiology Societies released recommendations to guide patients care, minimizing and delaying not necessary procedures and in-office visits.
Authors suggested to consider three steps for the remote care and monitoring of heart failure patients:
Patients should also monitor daily weight, blood pressure, heart rhythm and heart rate and should be reminded to adhere to appropriate dietary and drug therapy. A video assessment is recommended to evaluate the jugular venous pressure and peripheral oedema.
HeartLogic is the unique multisensor algorithm that combines daily information from five physiological sensors to calculate the HeartLogic index to detect patient’s heart failure worsening.
Authors highlight that “This technology affords a provider advantage to intervene to further optimize heart failure management and potentially prevent a face-to-face visit or hospitalization. […] and its interpretation to be derived from a collaborative effort between heart failure and cardiac electrophysiology providers”
The tools available for remote heart failure monitoring are based on the principle that small changes in cardiac physiology precede the overt signs and symptoms of heart failure and they may prevent hospitalizations.
In conclusion in this extraordinary period characterized by social distancing, the appropriate use of these technologies may be a powerful tool to provide a remote and efficient management for heart failure patients
Case of the month
On October 2019, a 58 years-old man with dilated cardiomyopathy and 34% LVEF underwent implantation of Vigilant X4 CRT-D. The patient was enrolled in Latitude Remote Monitoring system and HeartLogic feature has been activated.
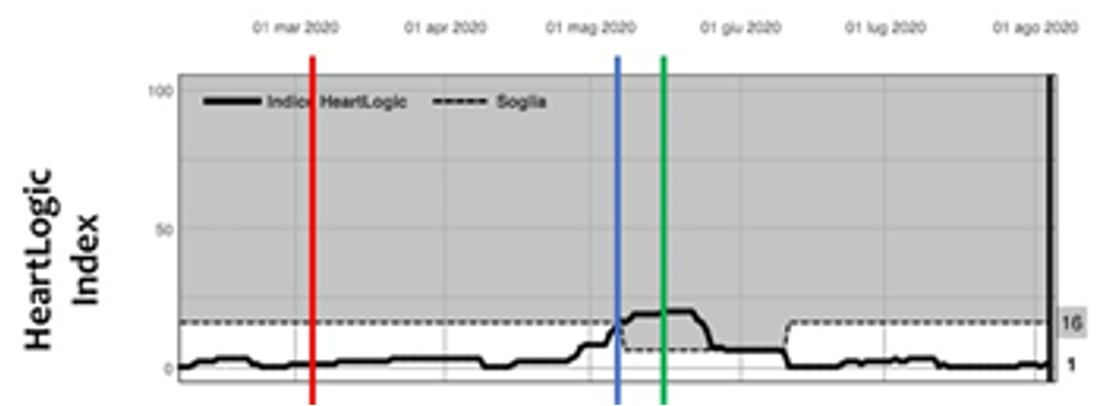
On March 3rd, 2020 (red line), at the beginning of COVID-19 pandemic in Italy…