Dear HeartLogic™ users,
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has infected more than 35 million people globally, with more than 1 million deaths recorded by World Healthcare Organization as of Oct 12, 20201.
Now a second wave of COVID-19 is affecting European countries, and this requires renewed attention to protect the most fragile patients.
During the first wave, major scientific organizations identified patients with heart failure among those more vulnerable to the effects of COVID-19, i.e. high risk of infection and high risk of associated morbidity and mortality.
Moreover, the restrictions imposed by the stay-at-home dispositions and more difficult access to hospitals can lead to a lower quality of care with serious clinical consequences.
In this issue we would like to share with you an update on the guidance issued by international societies of cardiology and latest evidence of HeartLogic use in this critical period.
Updates from International Societies of Cardiology
The specific session on Chronic Heart Failure patients reported that “The risk of COVID-19 infection may be higher in Chronic HF patients due to the advanced age and presence of several comorbidities” and suggested to avoid hospital access for these patients in order to preserve them and HCPs from COVID-19 infection.
This guidance encouraged the use of remote monitoring for patients with cardiac implantable devices to replace in-office visits.
The Heart Rhythm Society, as well, issued its consensus report3 describing the impact of COVID-19 on cardiac arrhythmias and the guidance for managing electrophysiology activities (procedures, visits and cardiac device interrogation). Main emphasis was given to remote monitoring of devices.
In this paper authors recognized the direct risks due to COVID-19, infection-associated morbidity and mortality, and indirect risks due to reduction of care following the decrease of in-person visits and hospital access (social distancing).

The solutions proposed included the quick introduction of technologies suitable to provide remote assessment of heart failure clinical status.
“Available remote patient monitoring technologies like […] HeartLogic™ […] should be adopted quickly to provide better assessment of HF clinical status while maintaining social distancing through the performance of virtual visits. Such […] technologies may better allow clinicians to keep patients with HF safely in their homes and minimize the need for in-person hospital or clinic visits. These systems, accompanied by their dedicated cloud-based information management, are no longer the future but the present of improved HF care.”
HeartLogic & COVID-19 publications
In this tough period, the availability of validated tools to monitor the heart failure status of ICD patients is important. New evidence has been published on that.
In July, Dr. Heggermont5 published the first case report of an HF patient implanted with a dual-chamber ICD equipped with HeartLogic algorithm that experienced a COVID-19 infection (full information in HeartLogic Newsletter 5/2020).
Recently Dr. Egolum (The Heart Center of Northeast Georgia Medical Center) published on JACC Case Report the paper “Applications of the Multi-Sensor HeartLogic Heart Failure Monitoring Algorithm during the COVID-19 global pandemic”6. He described two cases of patients with advanced heart failure who were actively monitored through the HeartLogic algorithm to guide care and limiting the hospital access.
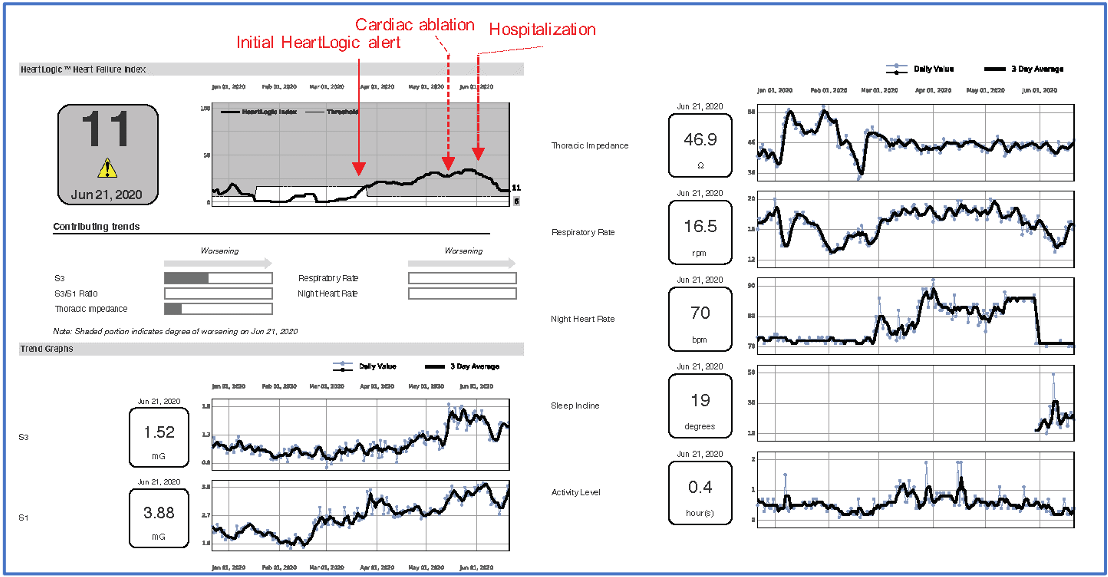
A 78-year-old man, implanted with CRT-D device underwent an atrioventricular junction ablation in mid-May. Some days after ablation the patient was still in HeartLogic alert status, led by S3, night heart rate and respiratory rate increases. Patient reported by phone weight gain and swelling, and physician decided to increase diuretic therapy. At the beginning of June a hospitalisation has been needed for intravenous diuresis and following decrease in HeartLogic index.
In figure 1 the HeartLogic and sensors trends were reported.
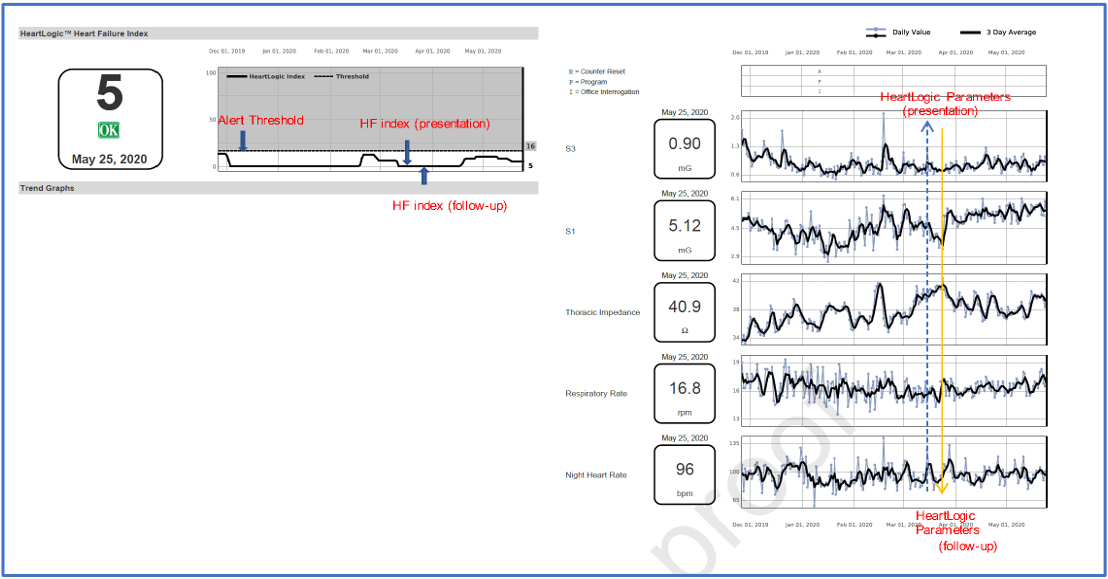
A 35-year-old man, with left ventricular assist device (LVAD) implant as bridge to decision and implanted with ICD device. During a video telehealth visit he reported dyspnea, orthopnea, cough and fatigue, but no apparent signs were observed (no jugular venous distension, no edema, abdomen non-distended) and patient refused face-to-face visit for concerns about COVID-19 infection. Any other signs of decompensation, device malfunction, arrhythmia have been detected at device interrogation and LVAD parameters were in normal range. All the HeartLogic index value were below the threshold, signifying a low risk of a HF event. The patient was reassured and no changes in drug therapy has been implemented. One week later a new telehealth follow-up was performed, and the patient was fine.
In Figure 2 the HeartLogic and sensors trends were reported.
The authors highlight the benefits from using the HeartLogic algorithm, and reported that it “provided critical data that expedited care delivery, allowed for appropriate triage of patients, with reduction in unnecessary clinic visits”
Another experience on the use of HeartLogic algorithm during COVID-19 pandemic was reported by Dr. Mitter (Zena and Michael A. Wiener Cardiovascular Institute, New York) in his publication “Insights from HeartLogic Multi-sensor Monitoring during the COVID-19 Pandemic in New York City”7.
This analysis examined 38 patients implanted with devices equipped with HeartLogic algorithm in the period before COVID-19 (February 2020) and during the stay-at-home orders (March-April 2020).
No difference in median HeartLogic scores was reported, even if a significant decrease in activity level and a corresponding drop-in mean heart rate have been observed. There was also a small increase in thoracic impedance value and, less frequently, in S3.
Authors concluded that, even if the sedentary behavior is supposed to be a driver to worsening heart failure status, the decreased autonomic tone may result in less congestion status and HeartLogic algorithm is able to detect this compensated situation without any alert occurrence.
These publications confirm HeartLogic as a valuable tool during this hard period of COVID-19 outbreak to maintain a constant heart failure status monitoring, to provide right care and, at the same time, to limit in-hospital accesses.
Case of the month

A 60 years-old woman underwent implantation of RESONATE™ X4 CRT-D in December 2018
In February, the patient underwent two ferric carboxymaltose injections because of iron-deficiency anemia, and concomitant increase in diuretic therapy was performed
At that time, the HeartLogic index was off, but…















