Dear HeartLogic™ users,
The Covid-19 pandemic has changed many of our habits, especially for in-person meetings and events. Virtual Congresses have quickly become “our new normal” by adapting their format, becoming more and more structured, accessible for sharing the latest findings in clinical practice.
The Annual Congress of the Heart Failure Society of America (HFSA 2020) has become the Virtual HFSA 2020 taking place from September 30th to October 6th.
https://hfsa.org/annualscientificmeeting
An Individualized, Alert-based Heartlogic Management Strategy Can Identify Patients At Risk For Impending Heart Failure Events
(A. Vigdor et al. – University of Pennsylvania, Philadelphia, PA) – POSTER SESSION
The MultiSense study has shown an alert threshold of 16 to be predictive of heart failure event (HFE), but there is currently no standard treatment protocol to manage these alerts.
The objective of this analysis carried out at the University of Pennsylvania (Philadelphia) was to assess the performance of HeartLogic alerts in predicting heart failure events among patients with chronic heart failure.
All patients with activated HeartLogic devices were prospectively followed for three months and monitored for HeartLogic alerts. Each alert was managed by phone assessment and diuretic changes were made based on the clinical team decision; a HFE was defined as an unscheduled visit of HF hospitalization occurring within 6 weeks after the initial alert.
A total of 80 patients were included in the analysis, and the details about alerts and HFE are reported in Figure 1
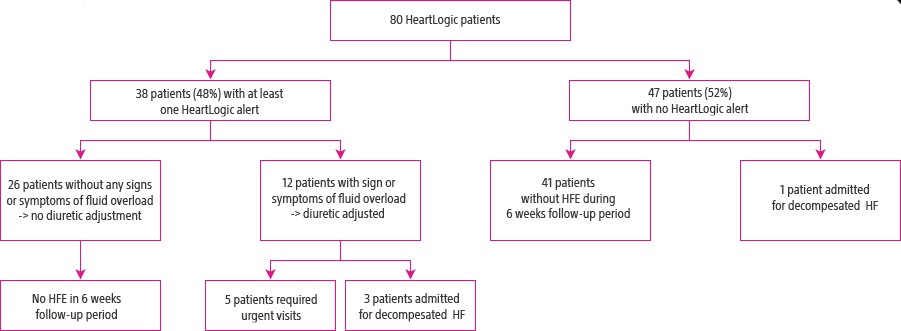
Overall, HeartLogic demonstrated:
- Sensitivity of 92%, Specificity of 61%,
- Positive predictive value of 32%
- Negative predictive value of 98%.
Increasing HeartLogic alert threshold to >20 in this cohort would improve specificity to 90% and positive predictive value to 56%, thereby reducing staff burden, with an acceptable sensitivity (69%) and negative predictive value (94%).
- This is the first study to evaluate the effects of an individualized HeartLogic threshold in an alert-based follow-up management strategy.
- Using an individualized HeartLogic threshold may improve specificity, consequently reducing staff burden.
Future studies are needed to determine if this management strategy leads to decrease in heart failure admission.
Remote Monitoring Of Heart Failure Using A Device-Based Multisensor Algorithm
(A. Chang et al. – VA Medical Center, Houston, TX) – POSTER SESSION
The purpose of this single center analysis was to evaluate if remote monitoring of CIEDs using the HeartLogic algorithm can lead to fewer total heart failure hospitalizations than remote monitoring of CIEDs without the HeartLogic algorithm.
This retrospective analysis was performed on 100 Boston Scientific devices not enabled with HeartLogic algorithm (implanted between 2015 and 2016) and on 40 HeartLogic enabled devices (implanted after 2017). All patients included in the analysis had chronic heart failure with an ejection fraction of no more than 35% on optimal medical therapy for at least 3 months (as defined by guidelines set by the American College of Cardiology).
For all patients, retrospective chart review was conducted for one year preceding and following device implantation, and the hospitalization rate for acute decompensated heart failure during these period was analyzed. When the HeartLogic index crossed a threshold, the information were reported to the clinic for further clinical evaluation.There were no differences between the two groups in terms of clinical baseline characteristics and drug therapy
| Standard ICD (n=100) | HeartLogic enabled ICD (n=40) | P value | |
| 1-year pre implant hospitalization | 33 (33%) | 17 (42%) | 0.33 |
| 1-year post implant hospitalization | 17 (17%) | 4 (10%) | 0.35 |
| Average number of hospitalizations | 1.94 | 1.5 | 0.56 |
Patients with HeartLogic-enabled devices showed a trend towards less 1-year heart failure admissions.
Additional studies are necessary to further evaluate this trend.
Multisensor Remote Monitoring For Heart Failure Exacerbations In Patients With Left Ventricular Assist Devices
(A. G. Hajduczok et al. – Penn State Hershey Medical Center, Hershey, PA) – POSTER SESSION
Continuous flow left ventricular assist devices (cf LVADs) have improved outcomes of advanced Heart Failure (HF) patients. Recurrent HF continues to be a complication and clinical examination is limited by the nature of the LVAD therapy requiring better diagnostics to improve patient outcomes.
This analysis, carried out on 2 LVAD patients, describes the performance of the HeartLogic feature and evaluates the correlation between S3 heart sound and clinically significant events.
- Events considered as clinically significant included:
- Driveline malfunction (requiring LVAD exchange)
- Invasive hemodynamic assessment to guide LVAD speed change
- Outpatient diuretic titration
Two patients with end-stage HF supported with a HeartMate II™ and HeartMate 3™ and implanted with a defibrillator enabled with a multisensor diagnostic for HF (HeartLogic) presented to clinic with exercise intolerance.
In both patients, exam revealed no elevation of venous pressure, lungs were clear, and no heart sounds were appreciated above the normal LVAD hum.
Both patients presented elevated filling pressures: LVAD speed was increased and consequently S3 magnitude decreased.
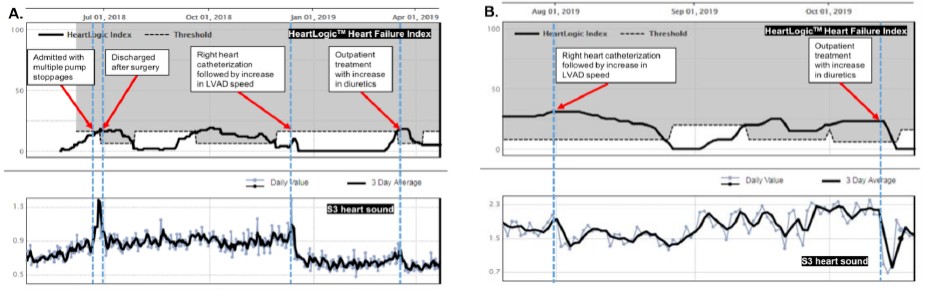
Later, patients experienced a total of five episodes of worsening heart failure associated with an increase in HeartLogic index and specifically, an increase in S3 heart sound. In each episodes the treatment led to a decrease in the HeartLogic value and in the S3 heart sound in manner consistent with the interventions that occurred, although clinicians could not appreciate an S3 through auscultation.
In figure 2, the five HeartLogic alerts, the S3 heart sound trends and the treatment provided were reported.
Clinicians typically have a difficult time appreciating any heart sound in LVAD patients. This is exacerbated by the loud, high-pitched machine noise associated with LVADs.The device-measured S3 is filtered to include only the 6-90 Hz frequencies, thereby removing much of the LVAD noise.
These cases demonstrate that the multisensor HeartLogic algorithm changes and alerts during clinically meaningful events, that is useful in the management of LVAD patients.
Comparison Of NT-proBNP Concentrations When In Or Out Of Heartlogic Alerts
(J. P. Boehmer et al. – MultiSENSE study group) – POSTER SESSION
This abstract was already presented at ESC-HF 2020 congress (HeartLogic newsletter 5/2020)
The objective of this analysis was to compare NT-proBNP concentrations during periods IN or OUT of an active HeartLogic alert.Out of a total of 855 valid NT-proBNP evaluations in 741 patients with valid associated HeartLogic index values, 180 NT-proBNP concentrations were measured while the HeartLogic state was IN alert and 675 NT-proBNP concentrations were measured while HeartLogic was OUT of alert.
When HeartLogic was IN alert, the NT-proBNP concentrations (6957.9±10398.0 pg/ml) were significantly higher than those when HeartLogic was OUT of alert (1675.5±4403.1 pg/ml) (p<0.001).
HF patients’ NT-proBNP concentrations were significantly elevated when HeartLogic was IN alert status, consistent with the HeartLogic algorithm capturing clinical worsening of HF status.