Case Study
By
Douglas G Adler MD, FACG, AGAF, FASGE
A 33-year-old man developed severe acute necrotizing pancreatitis of unclear etiology. The patient developed a large pancreatic fluid collection (PFC) largely replacing the body and tail of the gland. Biliary obstruction due to compression of the bile duct by the PFC was addressed by ERCP with plastic stent placement. Over 6 weeks, the patient’s PFC was seen to mature with good apposition to the posterior wall of the stomach. The patient was referred for EUS and transluminal stent placement/cystgastrostomy.
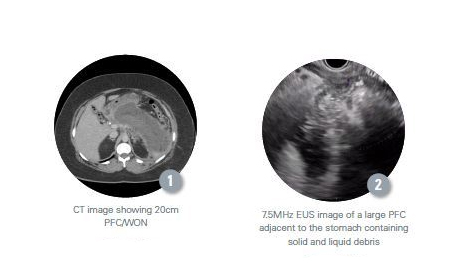
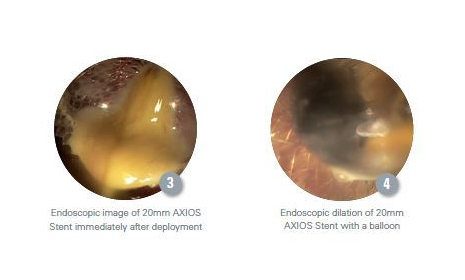
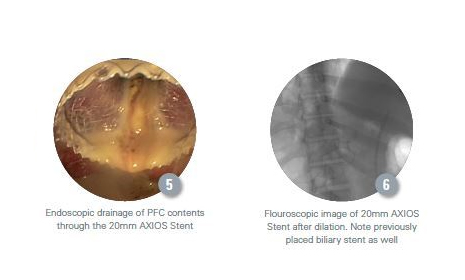
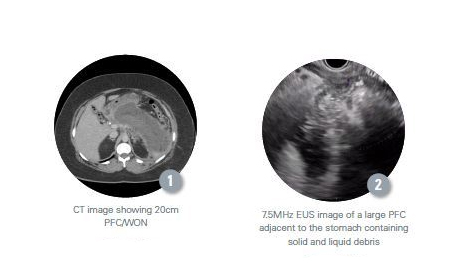
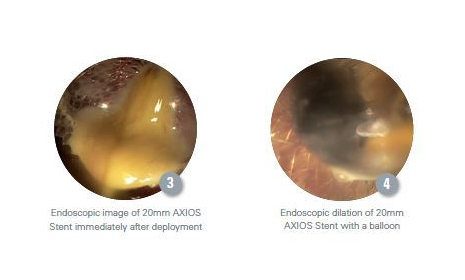
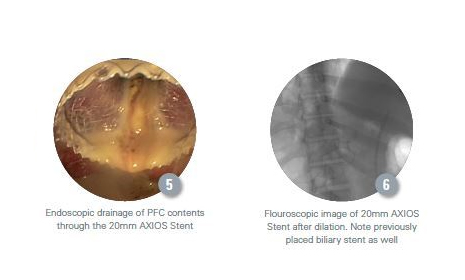
A 7.5MHz EUS with Doppler revealed a large PFC measuring 20cm (Figure 1). The lesion had a thick wall and contained copious solid and liquid debris (Figure 2), most consistent with walled-off pancreatic necrosis (WON). Using the AXIOS Stent, the PFC was accessed in a transgastric manner. A 20mm wide by 10mm long AXIOS lumen-apposing metal stent (LAMS) was deployed across the cystgastrostomy. (Figure 3) The AXIOS Stent was then dilated with an esophageal balloon to 15mm (Figure 4). Approximately 1L of purulent appearing, mixed solid and liquid PFC contents were seen to drain from the PFC to the stomach (Figure 5) and this was aspirated with the endoscope. The stent was left in situ (Figure 6).
Douglas G Adler MD, FACG, AGAF, FASGE
University of Utah School of Medicine, Huntsman Cancer Center, Salt Lake City, Utah, U.S.A.