How does cryoablation compare to partial nephrectomy?
Historically, the treatment for RCC was radical nephrectomy, but partial nephrectomy became the standard of care for small tumors as it preserves renal function and therefore delays or prevents initiation of hemodialysis.
More recently, tumor ablation, particularly percutaneous cryoablation, has emerged as an alternative to surgery in the treatment of RCC, especially for early stage (≤ 4 cm, localized) RCC tumors.
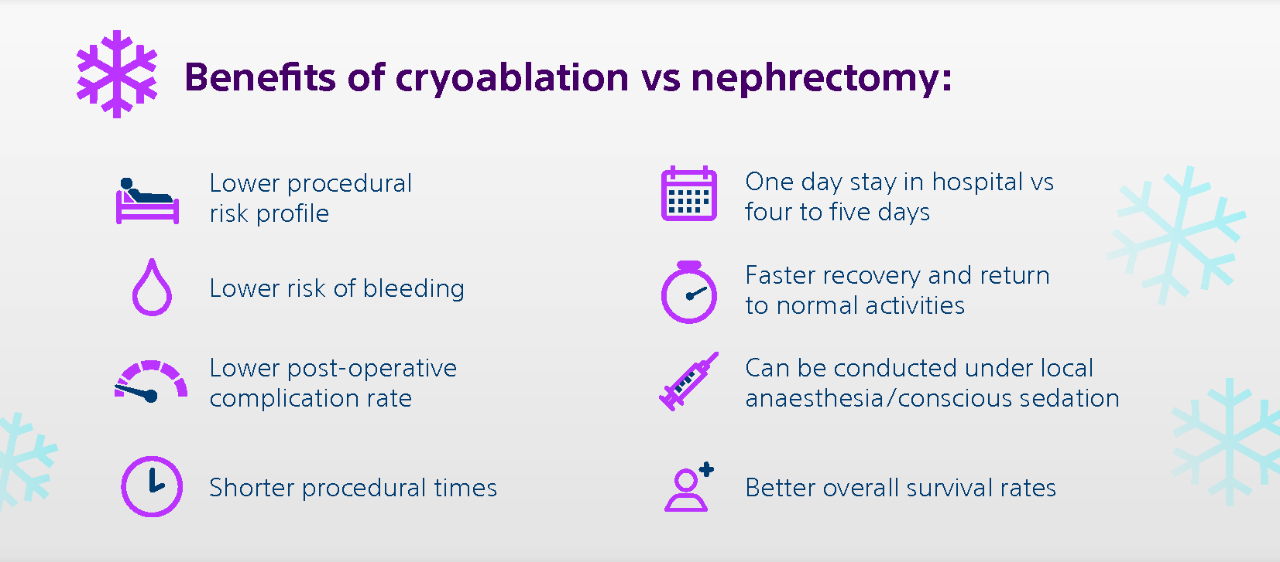
The marked increase in volume of percutaneous ablations offered to patients is likely due in large part to a growing body evidence demonstrating comparable oncologic outcomes with partial nephrectomy, but with decreased complications and preservation of renal function.[1]
When it comes to treating kidney diseases, in particular renal cell carcinoma, partial nephrectomy or nephron-sparing is considered the standard treatment.
However, in terms of effectiveness, cryoablation has demonstrated similar efficacy outcomes,[2] with similar local recurrence-free survival rates* and similar metastasis free survival rates.[3]
Cryoablation treatment is especially advantageous in patients with multiple comorbidities and technically complex lesions, who are not good candidates for surgery.
3 different studies[4,5,6] (single center, retrospective studies of T1A tumors) proved that cryoablation treatment showcased similar local recurrence free survival to partial nephrectomy.
Additionally, in a 10-years prospective study of percutaneous cryoablation for stage I renal cell carcinoma by Morkos et al (2020), the disease-specific survival was 94% at 5 and 10 years, equivalent to that reported after Radical Nephrectomy or Partial Nephrectomy.[1]
Cryoablation vs radiofrequency ablation
Both cryoablation and radiofrequency ablation are options for patients who decide to go for thermal ablation. Radiofrequency ablation (RFA) is a heat-based ablation technique.
The radiofrequency ablation technique uses high-energy radio waves to heat the tumor through a thin, needle-like probe placed through the skin and moved forward until the end of it is in the tumor. Placement of the probe is guided by ultrasound or CT scan. Once it is in place, an electric current is passed through the tip of the probe. The heat through the probe destroys the cancer cells.
Current data based on analyzing forty-seven studies representing 1375 kidney lesions treated by cryoablation or RFA, suggests that cryoablation provides superior oncologic outcomes. Cryoablation resulted in fewer retreatments, improved local tumor control, and it may be associated with a lower risk of metastatic progression compared with RFA.[7]
Cryoablation vs microwave ablation (MWA)
Microwave ablation (MWA) is one of the newer modality of thermal ablation and has proven its safety and efficacy in the management of the tumors amenable for ablation for primary and metastatic diseases. MWA uses microwaves to provide intense heat to destroy the tumor, while tissues with lower-water-content such as adipose tissues remain unharmed.
Cryoablation has certain procedural advantages over heat-based ablation techniques such as MWA and RFA. It allows the simultaneous use and synergy of more than one probe, thus sculpting the ice-ball.[7]
Cryoablation also has low intraprocedural pain as ice has an analgesic effect versus heat-based techniques which may cause significant pain. Moreover, the visibility of the iceball under CT guidance gives a better visualisation of the ablation zone. It also enables reliable efficacy evaluation as post-ablation boundaries following the procedure are smooth, uniform, and consistent with actual ablation. As compared to MWA that may cause irregular and unpredictable post ablation boundaries due to vascular heat sink effect and conductivity impact.
Clinical effectiveness of cryoablation and MWA are considered comparable, although long-term results (5 or 10 years) of MWA are not available.A meta-analysis of fifty-one studies representing 3950 kidney lesions showed there is no difference in local or metastatic recurrence between cryoablation and microwave ablation-treated small renal masses.[8]
1. Morkos J, Porosnicu Rodriguez KA, Zhou A, et al. Percutaneous Cryoablation for Stage 1 Renal Cell Carcinoma: Outcomes from a 10-year Prospective Study and Comparison with Matched Cohorts from the National Cancer Database. Radiology 2020; 296:452–459. doi: 10.1148/radiol.2020192325
2. Georgiades C. et al. Renal tumor ablation. Tech Vasc Interv Radiol. 2013 Dec;16(4):230-8.
3. Thompson RH. et al. Comparison of partial nephrectomy and percutaneous ablation for cT1 renal masses. Eur Urol. 2015 Feb;67(2):252-9.
4. Andrews JR, Atwell T, Schmit G, Lohse CM, Kurup AN, Weisbrod A, Callstrom MR, Cheville JC, Boorjian SA, Leibovich BC, Thompson RH. Oncologic Outcomes Following Partial Nephrectomy and Percutaneous Ablation for cT1 Renal Masses. Eur Urol. 2019 Aug;76(2):244-251. doi: 10.1016/j.eururo.2019.04.026. Epub 2019 May 3. PMID: 31060824.
5. Breen DJ, King AJ, Patel N, Lockyer R, Hayes M. Image-guided Cryoablation for Sporadic Renal Cell Carcinoma: Three- and 5-year Outcomes in 220 Patients with Biopsy-proven Renal Cell Carcinoma. Radiology. 2018 Nov;289(2):554-561. doi: 10.1148/radiol.2018180249. Epub 2018 Aug 7. PMID: 30084744.
6. Lim E, Kumar S, Seager M, Modi S, Mandal I, Neves JB, Jones S, Tran MGB, Munneke G, Bandula S, Walkden M. Outcomes of Renal Tumors Treated by Image-Guided Percutaneous Cryoablation: Immediate and 3- and 5-Year Outcomes at a Regional Center. AJR Am J Roentgenol. 2020 Jul;215(1):242-247. doi: 10.2214/AJR.19.22213. Epub 2020 Apr 14. PMID: 32286877.
7. Maria T, Georgiades C. Percutaneous Cryoablation for Renal Cell Carcinoma. J Kidney Cancer VHL. 2015;2(3):105-113. doi: 10.15586 Fjkcvhl.2015.34
8. Martin J & Athreya S. Meta-analysis of cryoablation versus microwave ablation for small renal masses: is there a difference in outcome? Diagn Interv Radiol. Nov-Dec 2013;19(6):501-7. doi: 10.5152/dir.2013.13070.















