Calcium Prevalence
ROTAPRO™ Rotational Atherectomy Systems
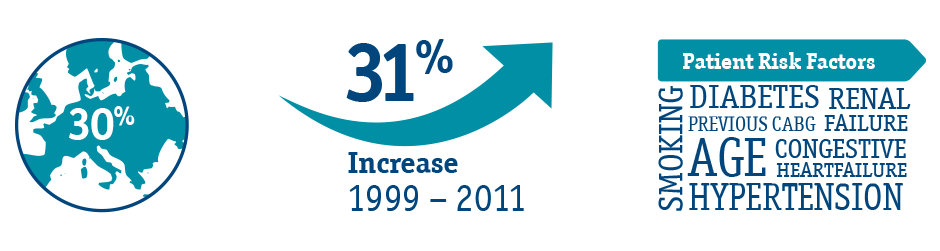
Over 30% of all patients treated for PCI present with some degree of calcium.1 This represents a 31% increase over the last two decades alone.
Patient complexity is increasing; risk factors such as an aging population, renal failure, hypertension, and an increasing prevalance of Type C lesions indicate that calcific lesions will continue to be present.1

Calcium Can Present Complications

Calcium is a Predictor of Worse Outcomes
Calcific CAD Treatment Options
Treat with Rotational Atherectomy
Identification is not the only area in which the status quo has failed to keep pace with your needs. POBA, a commonly used solution for addressing these lesions, can lead to dissections or perforations, leading to longer case time and limiting options for completing the case.15
Rotational Atherectomy is the gold standard for addressing lesions with any level of calcification. Rotational Atherectomy is known to deliver exceptional outcomes, with multiple studies indicating that Rotational atherectomy results in high procedural success rates with acceptable short- and longer-term MACE rates considering the severity of patient and lesion characteristics.16-18
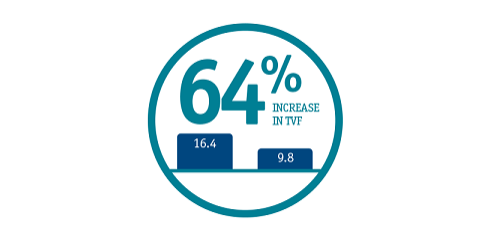
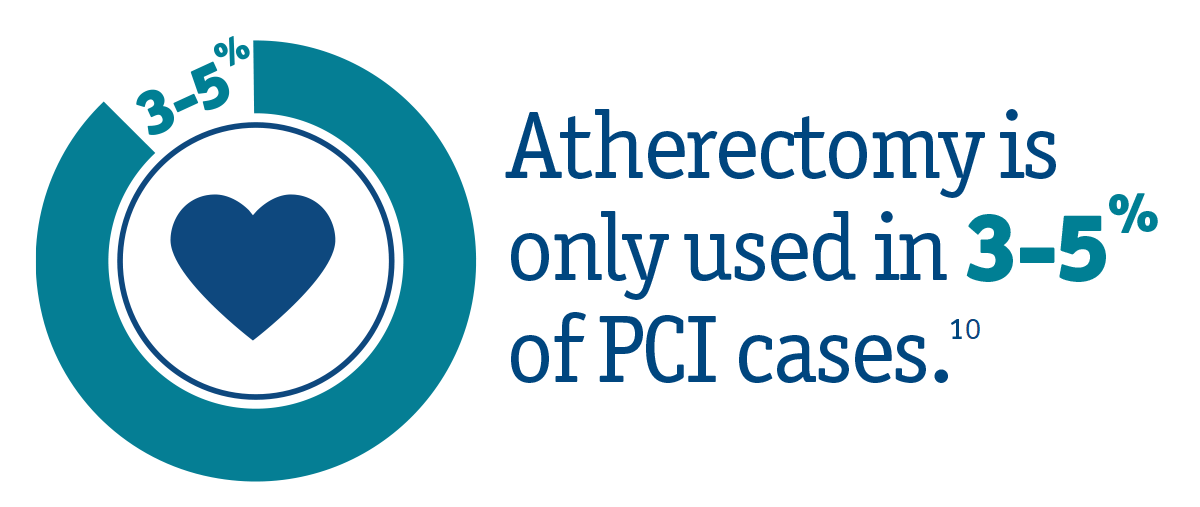
Calcium is being severely undertreated:

Atherectomy:
Gold standard treatment for Calcium
• Helps prevent complications and adverse events11
Diagnose with IVUS
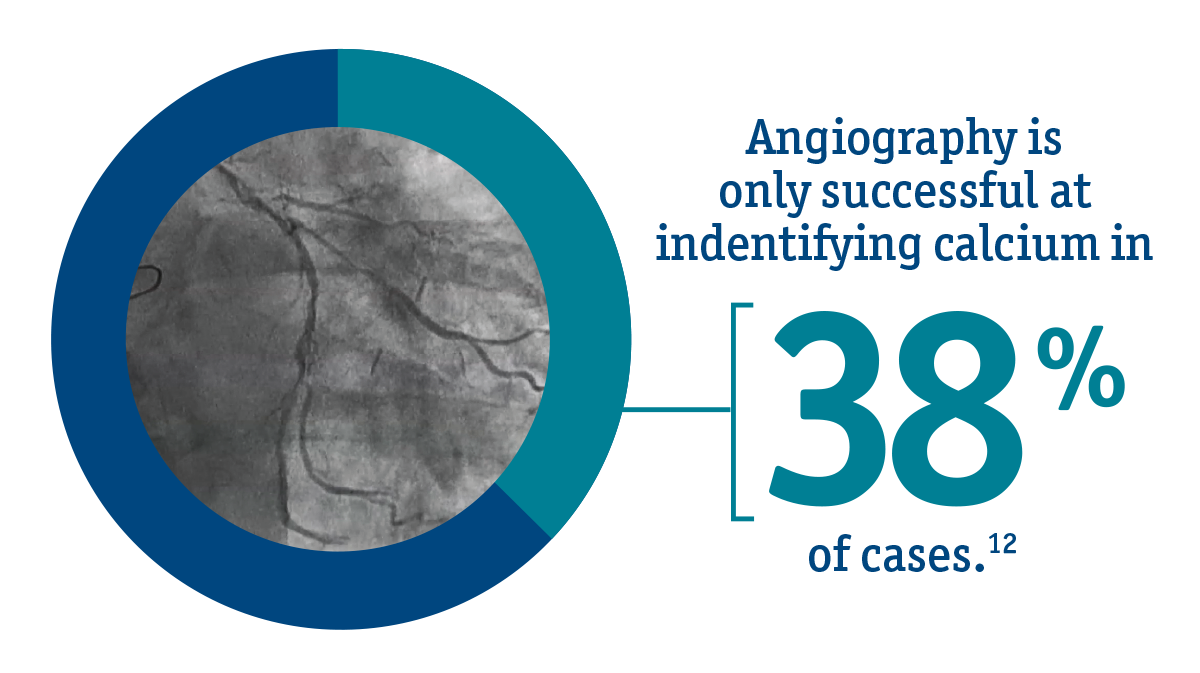
You can't treat what you can't see. Angiography is only effective at identifying the most severe cases of calcific CAD. In fact, only 38% of cases show visible calcium via angiography.12 Since low to moderately calcified lesions can still act as a considerable barrier to an optimal outcome, you'll need to use IVUS for every procedure.
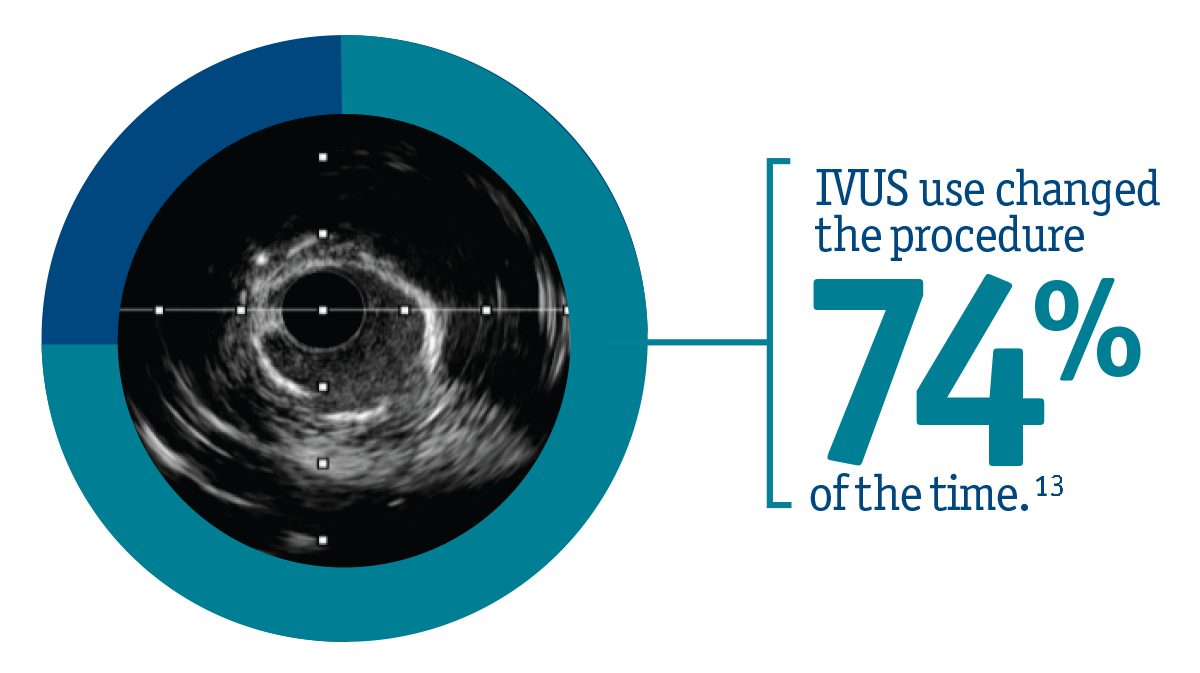
IVUS is the preferred option for effectively visualizing and identifying calcium, no matter the severity, allowing you to make better treatment decisions with confidence. In fact, the use of IVUS has been shown to change treatment decisions 74% of the time.13

IVUS is necessary for every procedure
• Allows for better treatment decisions