Dear HeartLogic™ users,
We hope that the emergency due to Covid-19 is solving and that your centers are going to recover a peaceful situation. We are grateful for your extraordinary commitment in this difficult period to ensure the best standard of care for all your patients.
Some restrictive measures have been put in place to stem Covid-19 and to protect the most fragile patients by reducing hospital access and encouraging the use of remote tools to monitor patient conditions. Heart Failure patients need continuous monitoring of their status in order to put in place prompt actions to manage possible worsening of heart failure condition. During this period HeartLogic™ may represent an aid for the early detection and management of impending heart failure events.
In this issue we would like to review with you the suggestions provided by the main cardiovascular associations for the management of heart failure during Covid-19 pandemic.
Covid-19 and Heart Failure
ESC Guidance
“The European Society of Cardiology (ESC) has assembled a group of experts and practitioners with experience in the care of COVID-19 patients to provide a guidance document relevant for all aspects of CV care during the COVID-19 pandemic.”
This document doesn’t replace the official ESC guidelines, but it reports only some recommendations to manage the patients with cardiovascular disease during this pandemic period.
The patients with cardiovascular disease who develop a COVID-19 infection have a higher risk of negative outcome. This is the reason why they should be protected from the exposition to COVID-19 and hospital access: elective procedure should be avoided, as possible, and the follow-up of patients should be performed through the use of telemedicine, especially for vulnerable groups. Telemedicine and home care are currently the best solution to prevent unnecessary hospital access and possible contact with infected subjects.
The use of telemedicine is recommended for continuous monitoring of stable patients and facilitates also the possibility of consultation with different specialists providing to the patients a complete approach to their disease without access to the hospital.
Remote monitoring of cardiac implantable devices is also strongly recommended and it should replace as much as possible all in-office visits. For patient not followed remotely, the remote monitoring activation should be considered, especially for Boston Scientific and Abbott devices that didn’t required any in-office visit for activation.
Urgent in-office visits or ambulatory device interrogation should be considered only for patients with suspected severe lead dysfunction, battery depletion (especially in PM-dependent patients), malignant arrhythmia detection and appropriate or inappropriate ICD therapy delivery.
HRS Guidance
The guidance suggests to postpone the non urgent or elective procedures that are unlikely to directly impact patients clinical care or outcomes in the next few months.
It is recommended, if possible, to avoid in person visits or follow-ups and to adopt telehealth or virtual visits, especially for low-risk patients as patients without symptoms suggesting worsening of heart failure or arrhythmia burden. By contrast, in-office visits are indicated for patients with worsening heart failure or arrhythmias symptoms, or for patients requiring device reprogramming.
In-office follow-up of implantable devices should be avoided, if it is not necessary, and the remote monitoring should be considered in order to reduce the need for non urgent clinic visits (Figure 1).
The Guidance reminds that, although remote monitoring is in class I recommendations, it is significantly underused because of a variety of patient- and system-based issues.
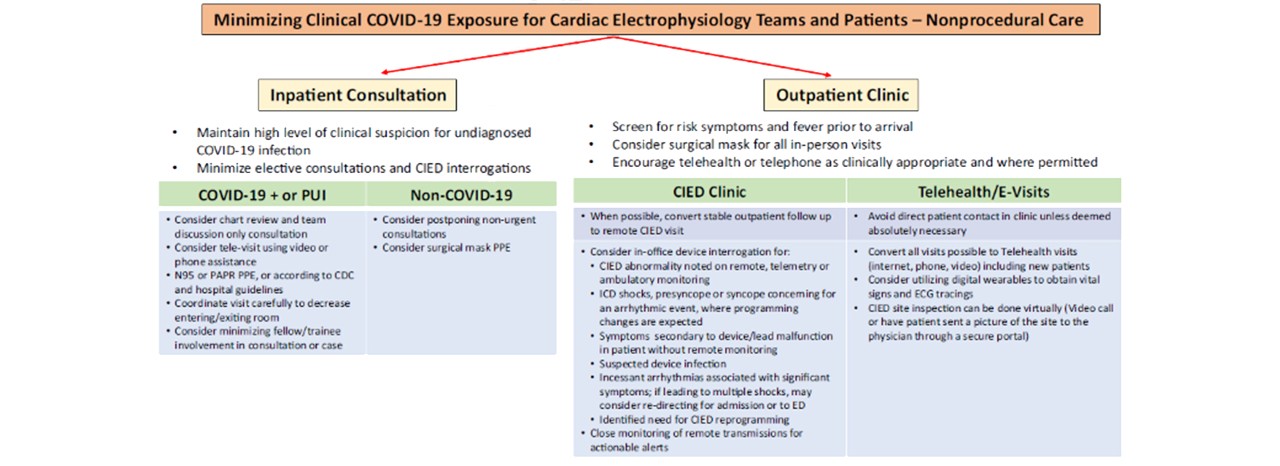
*PUI: Patient Under Investigation for COVID-19
The telemedicine and remote monitoring is strongly recommended as valuable resource also in the Guidance for rebooting electrophysiology through the COVID-19 pandemic from HRS and AHA society.
In regions with high COVID-19 burden, in-person clinic visits may still need to be minimized, using telehealth options for patients monitoring.
The remote monitoring of implantable device is still recommended and should be considered also for patient who are currently not enrolled.
Covid-19 in HeartLogic patient
It’s a pleasure to share with you the first publication about the HeartLogic™ index and COVID-19 pandemic by Dr. Heggermont from Cardiovascular Research Center of OLV Ziekenhuis, Aalst ( Belgium).
This case report is about an HF patient implanted with a dual-chamber ICD equipped with HeartLogic™ algorithm that experienced a Covid-19 infection.
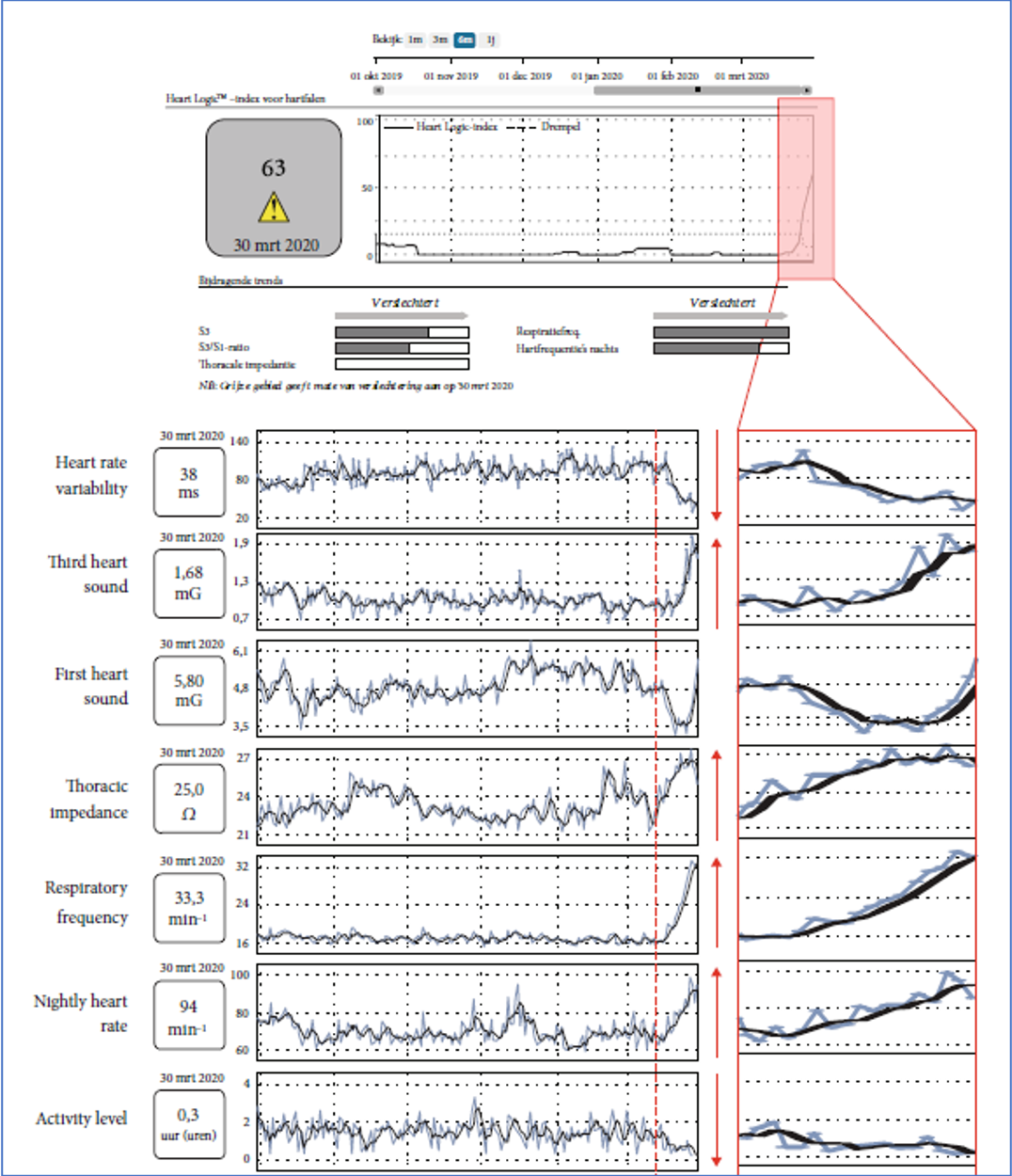
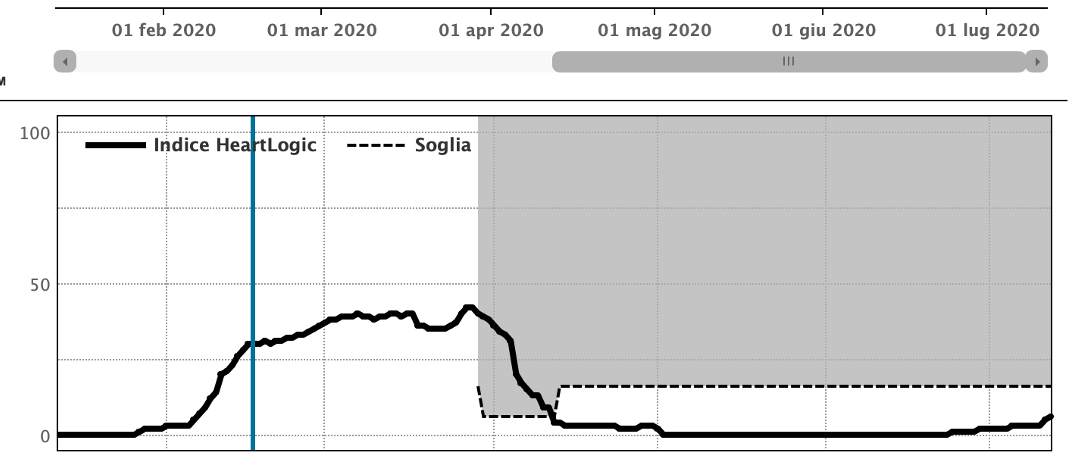
The sensors trends analysis shows that the main contributor to the HeartLogic™ alert is provided by respiratory rate, but also heart sounds and night heart rate are involved in index increase. The thoracic impedance instead showed an increased trend that is very atypical in heart failure decompensation.
The increase in respiratory rate and contextual increase in thoracic impedance are in contrast with pure heart failure events that usually leads a fluid overload. The authors hypothesize that “the increase in thoracic impedance might be explained by multiple factors, e.g., strongly increased respiratory frequency and air trapping due to hyperinflation“
According to the authors, the parameters that contributed to the alert helped to differentiate COVID-19 from heart failure exacerbation.
Discrimination between “typical” and “atypical” alert patterns might allow early detection of heart failure events and events of different origin, like SARS-CoV-2 infection.
Case of the month
An 87-year-old woman underwent implantation of Vigilant X4 CRT-D for primary prevention of sudden cardiac death on February 20th, 2018.
During the Covid-19 pandemic the center decided to activate HeartLogic™ index in heart failure patients in order to ensure continuous monitoring even in the lockdown period.
The HeartLogic™ index was finally activated on March 29th 2020 and the physician became aware...