Medical Specialties > Interventional Cardiology > Coronary Interventions > Clinical Data > Coronary Physiology > Fractional Flow Reserve (FFR)
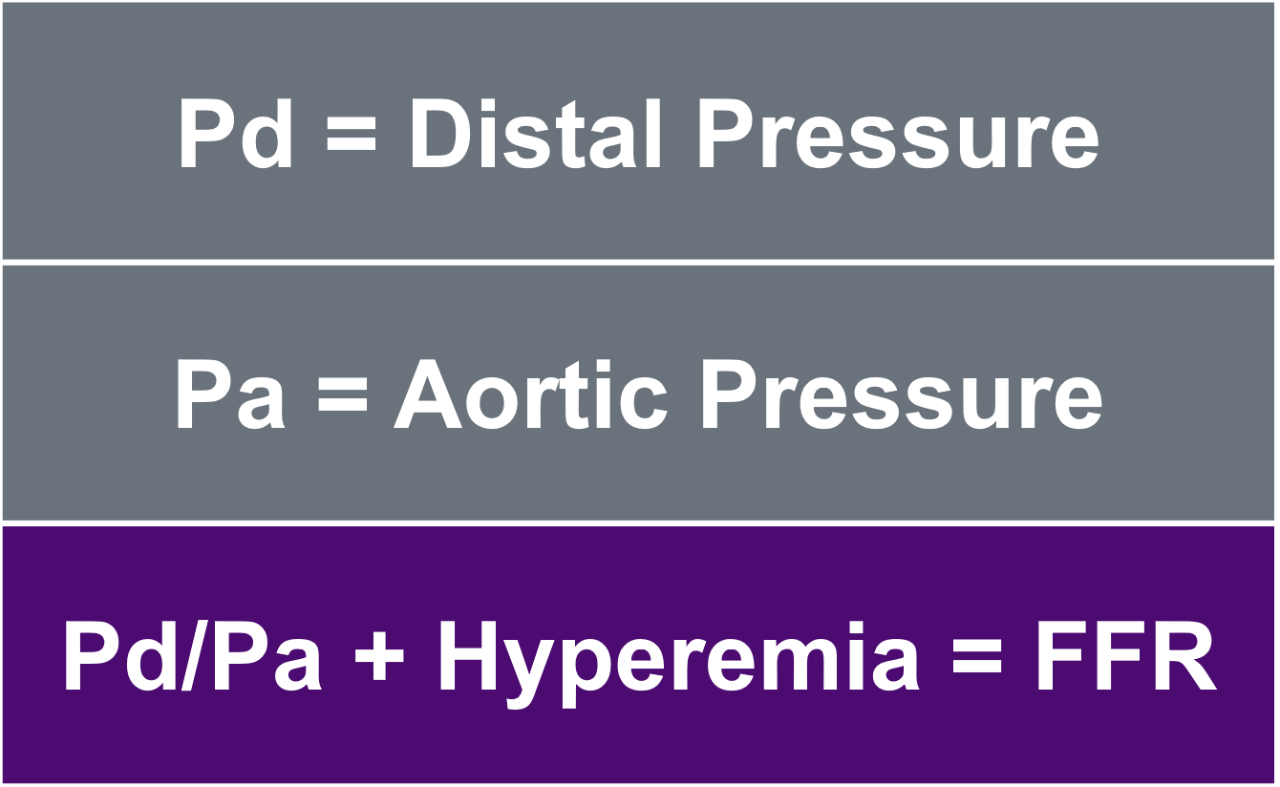
What is Fractional Flow Reserve (FFR)?
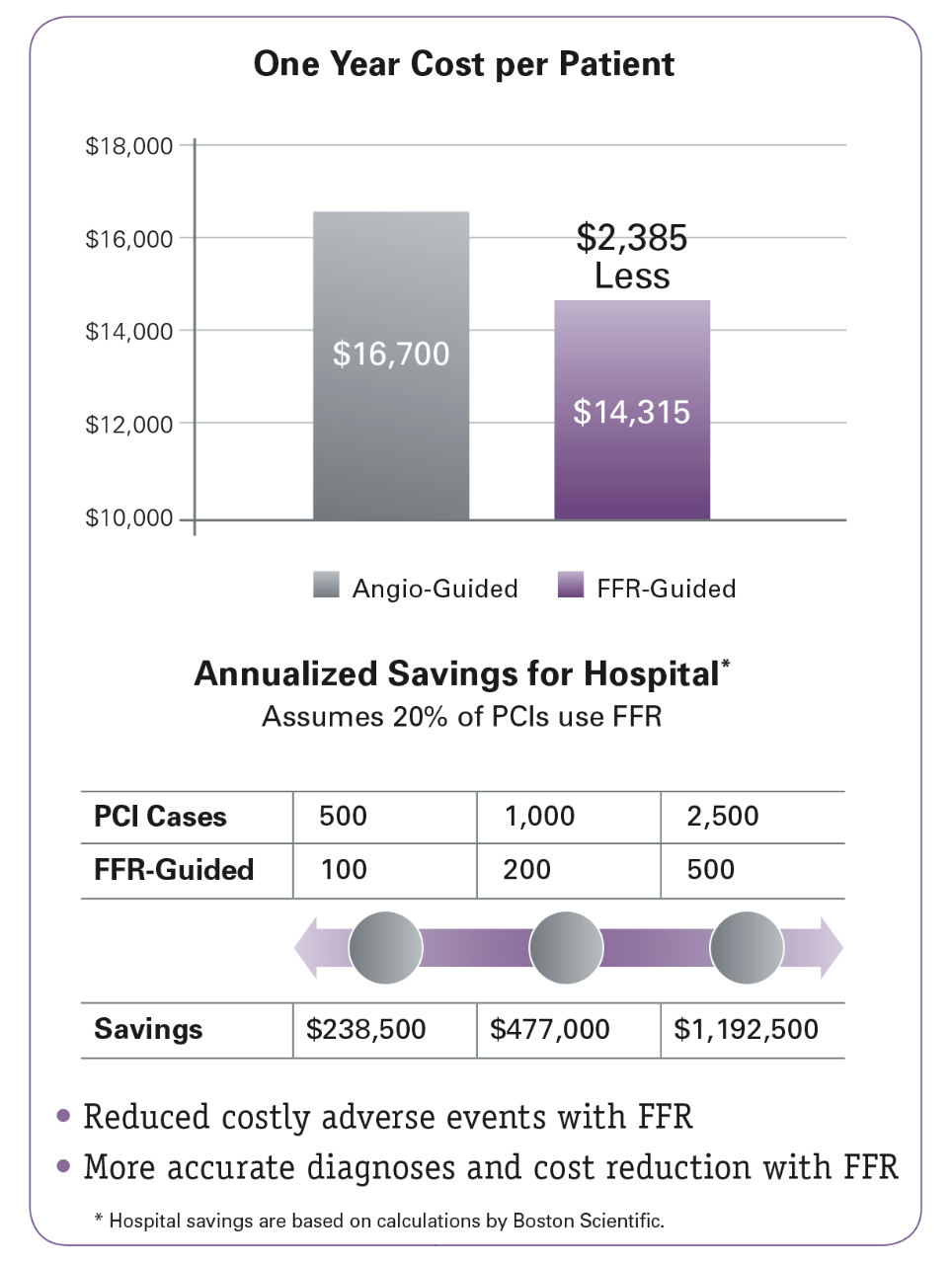
- Savings of $2,385/patient over one year in patients with multi-vessel disease.5
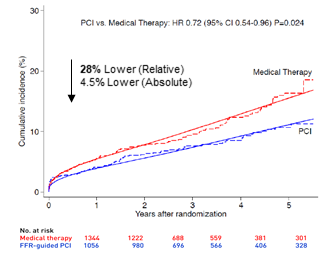
- FFR use demonstrated improved overall health outcomes at one year with less MACE, MI, and death.5
Learn how to optimize your approach with IVUS and the POLARIS Multi-Modality Guidance System.
See the broadest portfolio of dependable, sophisticated PCI devices.
Get exclusive product updates, training and educational opportunities, and more.
Fill out a quick form and one of our sales representatives will be in touch.